Case Presentation: Superior mesenteric artery syndrome is a rare condition characterized by symptoms resulting from vascular compression or obstruction of third part of duodenum in the angle between the aorta and the superior mesenteric artery. It has an estimated 0.013–0.3% prevalence (1)
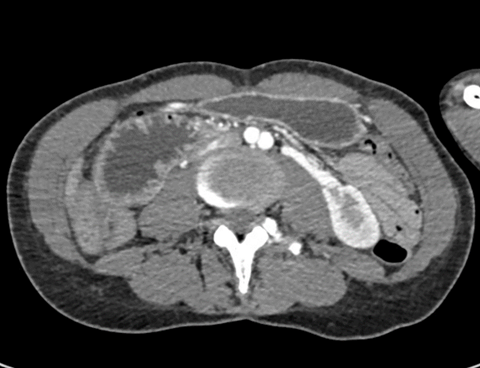
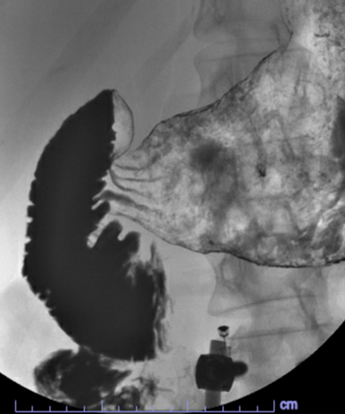
Discussion: A 30-year-old woman presented to the emergency department with epigastric abdominal pain, intractable nausea and multiple episodes of vomiting. She also reported severe, cramping, non-radiating epigastric pain of one week duration and multiple episodes of vomiting (8 times a day) 3 days prior to presentation. She is a chronic heroin user who last used heroin about one week prior to presentation. History revealed significant weight loss (100 pounds in the past year) with similar episodes of epigastric pain during that period of time. On examination, she was chronically ill appearing and cachectic with sunken eyes. Her vitals were within normal limits. She had severe epigastric tenderness on superficial palpation.Her labs revealed an elevated creatinine of 1.4 from a baseline of 0.6,blood urea nitrogen (BUN) of 32 and a bicarbonate of 28. After intravenous fluid hydration her creatinine improved to 0.83, BUN to 28 and Bicarbonate to 22. Lipase was 75. Liver function tests were normal. White blood count was 13.2 X 109/L, hemoglobin was 15.8 gm/dL and MCV was 77.5. Her urine drug screen was negative.She was initially managed symptomatically with IV hydration and anti-emetics, however due to persistent severe pain and the patient’s history of similar episodes in the past, an obstructive pattern was suspected. A CT scan of the abdomen showed a grossly distended stomach and duodenum with intraluminal fluid and abrupt tapering of the intestine at the level of the superior mesenteric artery (SMA) just right of midline shown in the images below with the aortomesenteric angle being around 20 degrees and then aortomesenteric distance being around 6 mm. Further evaluation with GI fluoroscopy showed compression of the transverse duodenum by the SMA causing intermittent obstruction and dilatation of the proximal duodenum which confirmed the diagnosis of superior mesenteric artery syndrome. A few hours later she developed chills, flushing and increased restlessness which raised concern for opioid withdrawal symptoms as well. During her admission she was treated symptomatically with pain management, IV fluids with increased focus on gradually increasing her calorie intake and nutritional supplementation. She was discharged home and was asked to follow up as an outpatient to ensure weight gain and symptom resolution.
Conclusions: Drug abuse has been reported in the literature as one of the causes of SMA syndrome. A good history and high index of suspicion increases the chances of making the diagnosis in this group of patients. 2 The long-term prognosis in people with SMA syndrome varies and depends on how much the syndrome has progressed. One of the main goals of treatment is prevention of bowel ischemia as soon as possible to help decrease the mortality rate. Confirming the diagnosis as quickly as possible and starting appropriate treatment decreases the chance of complications. The mainstay of the treatment for those presenting with symptoms less than a month is conservative management with fluid and electrolytes to correct electrolyte imbalances along with providing nutritional support with hyperalimentation for weight gain.3,4