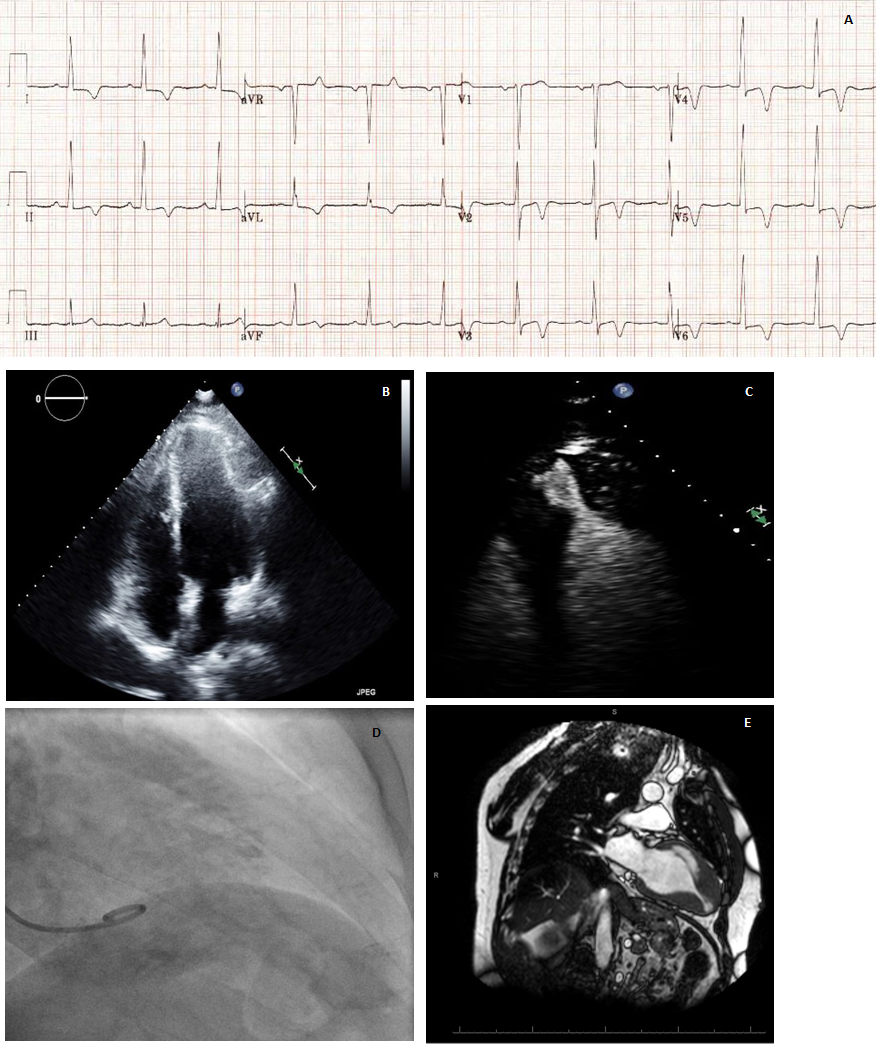
Case Presentation: 49 year old Caucasian male was admitted to the hospital after suffering an outside hospital cardiac arrest due to ventricular fibrillation. His electrocardiogram (EKG) showed findings of left ventricular hypertrophy (LVH) with giant T wave inversions in anterolateral leads (fig A). An Echocardiogram showed ejection fraction of 65-70% with moderate concentric LVH and apical hypertrophy (fig B) with focal outpouching of apex seen with contrast injection (fig C). He underwent cardiac catheterization which showed long tubular apex (fig D) with a gradient without significant coronary artery disease. Cardiac MRI showed small left ventricular (LV) cavity, marked hypertrophy of apical segments with a classic spade shaped appearance in diastole, thinned and dyskinetic LV apex and transmural scar of LV apex likely representing autoinfarction of apex (fig E). A diagnosis of apical hypertrophic cardiomyopathy (HCM) was made. He subsequently underwent implantation of single chamber Implantable Cardioverter Defibrillator (ICD) for secondary prevention of cardiac arrest and was discharged on beta blockers.
Discussion: Apical HCM is an uncommon variant of HCM which is localized to the left ventricular apex with or without midsegment involvement and with or without an apical aneurysm. It is more common in Japan and rare in United States with reported prevalence of 1-3%. Most patients are asymptomatic although they may also present with angina, heart failure (from diastolic dysfunction), myocardial infarction or arrhythmias. Features of classic HCM like LV outflow tract obstruction and mitral regurgitation are absent. Apical HCM can be diagnosed based on multimodality imaging. ECHO shows hypertrophied LV apex with wall thickness > 15 mm. Cardiac MRI shows typical spade like configuration of LV cavity at end diastole. Unlike classic HCM, apical HCM is usually not associated with sudden cardiac death and is believed to have a benign prognosis in terms of cardiovascular mortality. We report a case of cardiac arrest in apical HCM due to ventricular arrythmia. Cases of apical HCM should be evaluated for risk factors of sudden cardiac death (non sustained ventricular tachycardia, family history of sudden cardiac death, syncope, LV apical aneurysm and late gadolinium enhancement on MRI) and ICD should be considered in the presence of these risk factors. Beta blockers are the initial drugs of choice and non dihydropyridine calcium channel blockers (verapamil, diltiazem) can be added if beta blockers are ineffective or not tolerated. Role of anticoagulation for apical HCM patients with apical aneurysm is not clear.
Conclusions: Apical variant of HCM is an uncommon variant of HCM that is believed to have a benign prognosis. However, ventricular arrhythmias do occur in a subset of these patients leading to cardiac arrest. Patients with apical HCM should be evaluated for risk factors of sudden cardiac death and ICD implantation should be considered for high risk features. Multimodality imaging is of value in identification of these high risk features.