Background: Cardiac arrhythmias pose a significant risk to hospitalized patients, with the potential for increased morbidity and mortality. Rapid recognition of clinically significant arrhythmias is crucial for timely intervention. Cardiac telemetry monitoring offers a means of remote heart rhythm surveillance in the hospital setting. However, limited availability of telemetry beds in many hospitals and the overuse of telemetry can lead to prolonged emergency department stays for patients awaiting telemetry beds. Moreover, excessive telemetry use contributes to alarm fatigue and diverts nursing resources from more critical patients.
Purpose: Our project aimed to address these challenges by improving the appropriate utilization of cardiac telemetry in hospitalized patients. Specifically, we sought to identify patients who no longer required arrhythmia monitoring and discontinue telemetry orders for these patients. We hypothesized that clinicians were not consistently adhering to evidence-based guidelines for cardiac telemetry monitoring in hospitalized patients. Our goal was to increase the percentage of patients with discontinued telemetry orders before discharge by 10% in a designated telemetry unit within a period of four months.
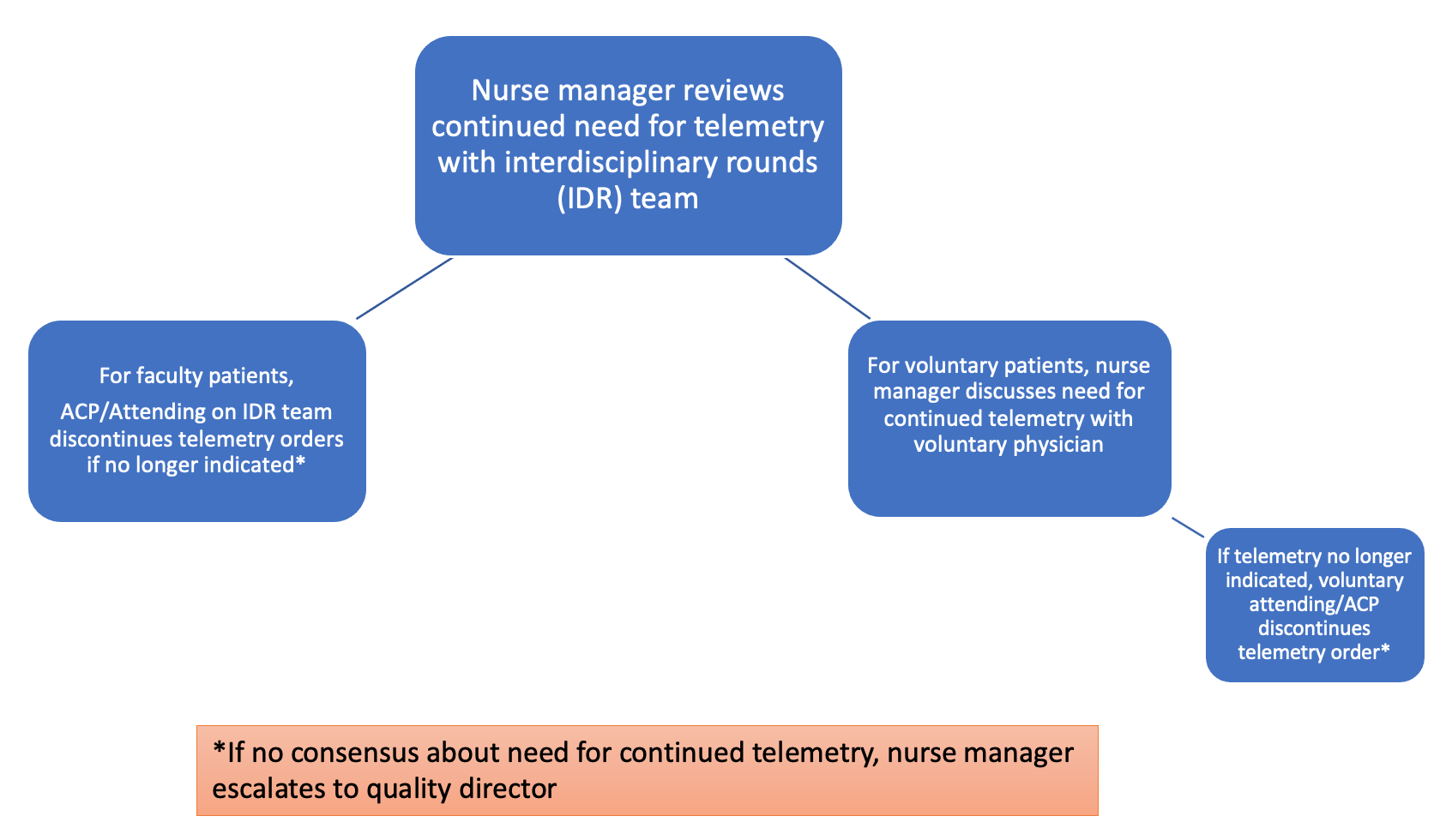
Description: To achieve our goals, we formed a multidisciplinary team comprising the director of inpatient quality, hospitalist physicians, advanced care practitioners, nurses, nurse managers, and telemetry technologists. The project received support and mentorship from the institution’s chief executive officer and medical director.The team undertook several key steps:- Collaborated with nursing and physician leadership on a medical ward with telemetry capabilities to identify patients no longer needing telemetry monitoring- Conducted a literature review to identify evidence-based guidelines for electrocardiographic monitoring in hospitalized patients, as published by the American Heart Association, and distributed these guidelines to unit physicians and advanced care practitioners- Developed and implemented a telemetry discontinuation pathway to address instances where attending physicians disagreed with telemetry guidelines (Figure 1)- Monitored telemetry discontinuation rates monthly
Conclusions: The results of our project demonstrated an increase in telemetry discontinuation rates from 44% to 47.8% after the educational intervention, although the rate remained below the hospital average (48.5%). Implementation of the escalation pathway resulted in a further increase in telemetry discontinuation rates to 54.2%, still slightly below the hospital average (56.7%). The escalation pathway, while valuable, was not the sole factor contributing to this increase. Awareness of the pathway may have led to more judicious use of telemetry by providers, and interventions by senior hospital leadership during patient surges also played a role.Our project offers a framework for identifying and addressing inappropriate cardiac telemetry utilization. It highlights the importance of assessing the use of evidence-based guidelines and involving essential stakeholders in determining ongoing telemetry needs. Challenges encountered included misconceptions about the benefits of telemetry monitoring and unclear clinical indications. Future steps may involve engaging cardiologists to provide expert guidance on arrhythmia monitoring and seeking support from hospital executive and medical leadership to sustain and expand the intervention.