Background: Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), constitute a major health problem in the United States Health System, with a reported high mortality rate and significant economic toll. Despite the prevalence of VTE and associated mortality, clinicians have struggled in prescribing appropriate VTE prophylaxis for the inpatient population, often over or under prescribing, subsequently increasing patient risk, compliance, and cost.
Methods: Resident admissions at Abbott Northwestern Hospital, Internal Medicine Residency, on each Wednesday from February 17, 2019 to July 17, 2019 were evaluated for appropriate selection of VTE prophylaxis. Rates of appropriate prophylaxis, frequency of inappropriate SCD use, subcutaneous heparin or enoxaparin use, and lack of VTE prophylaxis were then compared both pre and post-intervention. Interventions included a formal presentation to resident physicians on the use of the Padua, IMPROVE, and IMPROVE Bleed scoring systems in making appropriate selection, as well as the implementation of a VTE prophylaxis tool to allow for quick and easy interpretation of VTE risk. Appropriate selection was determined using the Padua, IMPROVE, and IMPROVE Bleed scoring systems in a retrospective chart review.
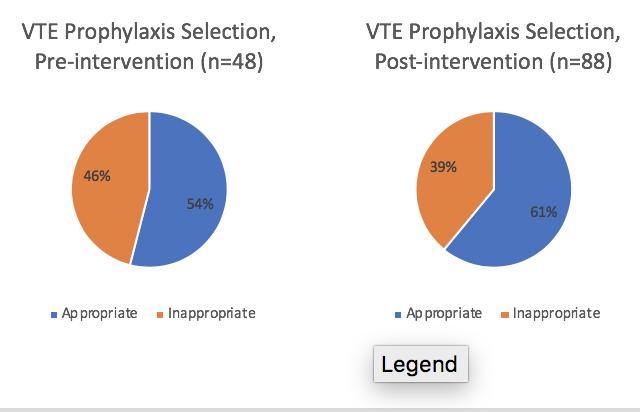
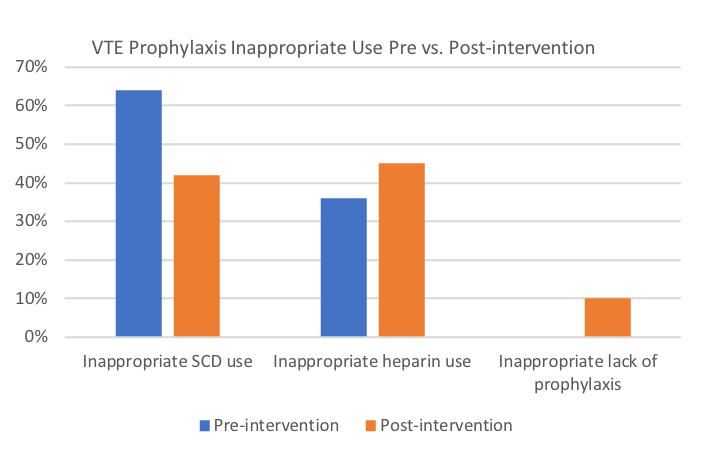
Results: Our results showed an overall increase in appropriate VTE prophylaxis rates from 54% to 61% following intervention. Inappropriate use of SCD’s dramatically improved from 64% to 42% with the caveat that inappropriate use of subcutaneous heparin and inappropriate lack of prophylaxis rates increased from 36% to 45% and from 0% to 10%.
Conclusions: Our data shows a clear improvement in appropriate prophylaxis use following instruction and awareness, however, heparin and lack of prophylaxis are still being used inappropriately. Further interventions include implementing the Padua and IMPROVE scoring system into the admission order set, as well as further teaching interventions. With increased awareness, and appropriate selection of VTE prophylaxis, we hope to decrease patient risk for VTE while inpatient while minimizing both VTE prophylaxis related complications and cost during hospital admission.