Background: Pregnant patients labeled with a penicillin allergy (PcnA) and charted as Group B streptococcus (GBS) positive can spread this infection to their baby during a vaginal delivery resulting in serious illness for their newborns. GBS is the most common cause of infectious morbidity and mortality in the neonatal period during the first week of life known as early-onset neonatal GBS disease (1). Prophylactic antibiotics given intrapartum have reduced the incidence of early-onset neonatal GBS disease by 70% (2, 3). Patients labeled with PcnA receive either vancomycin or clindamycin as an alternative prophylaxis to penicillin to prevent early-onset neonatal GBS disease but the effectiveness of this treatment is controversial (4, 5).
Methods: We collected retrospective data with institutional IRB approval from 2016 – 2018 for hospitalized pregnant patients who received antibiotic prophylaxis for GBS and were labeled as PcnA or non-PcnA. Statistical tests included calculations of means, medians, proportions, Mann-Whitney, two-sample t-tests, Chi-squared or Fisher’s Exact tests, and generalized linear and logistic regression models. Significance was set at p < 0.05. Inclusion criteria were GBS positive pregnant women who completed a vaginal delivery at our hospital. Exclusion criteria were age < 18 years old and did not consent to their health data used for research.
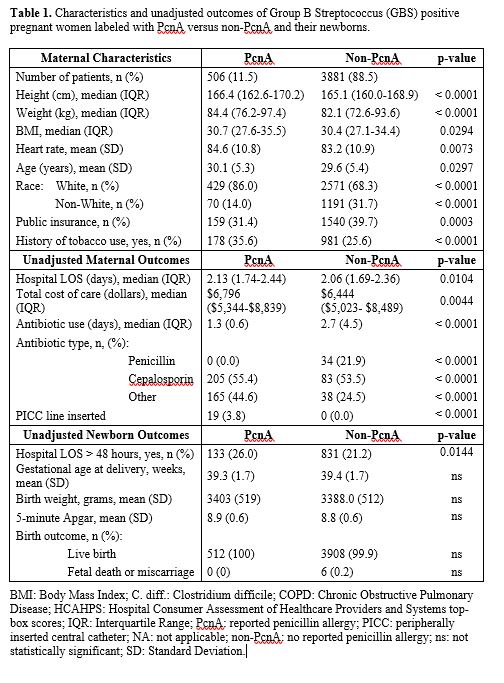
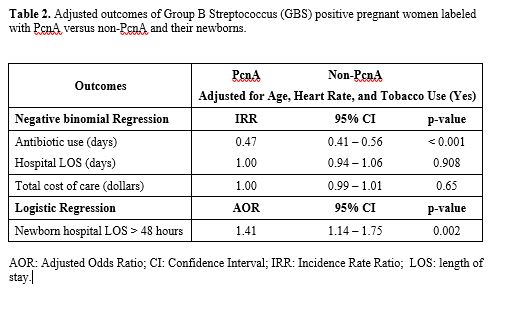
Results: We analyzed retrospective data from 4,387 hospitalized GBS positive pregnant patients of whom 506 (11.5%) had a PcnA label and 3881 (88.5%) did not. Pregnant women with a PcnA label were predominantly white, taller, had higher weight, BMI, mean heart rate, and age, and less public insurance coverage and tobacco use than pregnant GBS positive patients who did not have a PcnA label (non-PcnA) (p < 0.05, Table 1). For the PcnA group, unadjusted differences in patient outcomes included a longer mean hospital LOS (p = 0.0104), a higher total cost of care (p = 0.0044), a higher proportion of peripherally inserted central catheter (PICC) line use (p < 0.0001) and of newborn LOS being longer than 48 hours (p = 0.0144). The non-PcnA labeled women had a longer duration of antibiotic use (Table 1). When adjusted for age, pulse, and tobacco use, pregnant GBS positive women with a PcnA label had 53% fewer days of antibiotic use compared to not having a PcnA label (IRR: 0.47, CI: 0.41 – 0.56). When adjusted for age, race, and insurance category, pregnant GBS positive women with a PcnA label had higher odds of having a newborn whose hospital LOS was greater than 48 hours (AOR: 1.41, CI: 1.14 – 1.75). PICC line use was not included in the regression analysis because only 3.8% of the PcnA group and none of the non-PcnA group used them.
Conclusions: Group B streptococcal (GBS) infection remains the most common cause of neonatal early-onset sepsis and a significant cause of late-onset sepsis among young infants (6). Pregnant patients who are GBS positive with a PcnA label often receive GBS prophylaxis consisting of vancomycin or clindamycin. There is insufficient evidence to show that these agents are adequate in preventing early onset GBS (6). Our research found that this leads to a higher LOS and a higher total cost of care for these patients. De-labeling of a penicillin allergy is recommended by the AAP (6), and would likely lead to a lower LOS and total cost of care, and would ensure mothers and infants would receive the recommended treatment for GBS prophylaxis of cefazolin or a penicillin.