Background: Approximately 1.6 million men and 800,000 women in the US are alcohol dependent and have an alcohol-use disorder. Half will experience withdrawal symptoms after decreased alcohol consumption. Complications including seizures and delirium tremens occur in 3-5% . Benzodiazepines are the gold standard for treatment of alcohol withdrawal but choice of drug regimens varies widely. At a 12-hospital system in Minnesota, a symptom-based detoxification scale assessment tool (MINDS) and a single standardized high dose, diazepam-based treatment protocol (loading dose up to 80 mg diazepam) was initiated for alcohol withdrawal patients. Patient outcomes were assessed for MINDS use compared to use of older protocols administering lower initial benzodiazepine equivalents to diazepam doses (Pre-MINDS).
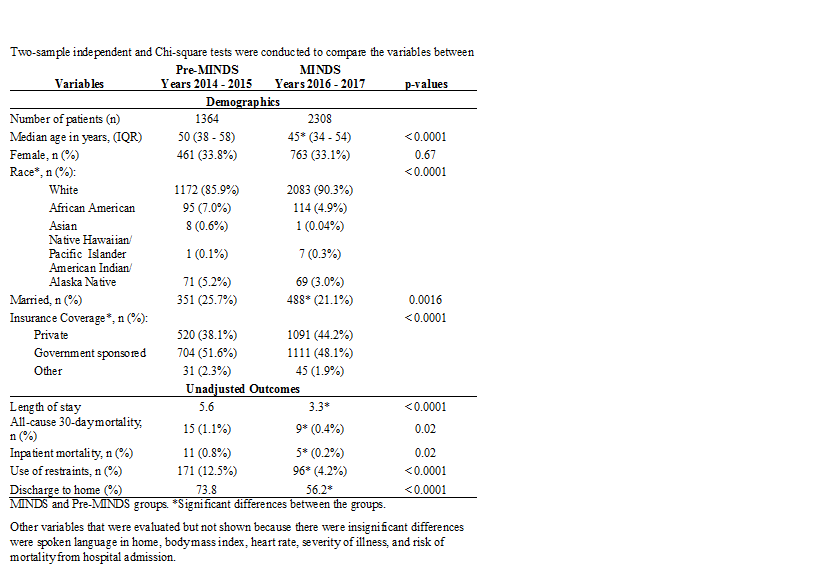
Methods: Retrospective data were collected from 2016 – 2017 for patients in the MINDS group (n = 2308) and from 2014 – 2015 for the Pre-MINDS group (n = 1364) and analyzed using Chi-square and two-sample t-tests, linear and logistic regression. Inclusion criteria were adult patients with an ICD-9 diagnosis of alcohol dependence or acute alcohol withdrawal, use of an order set for an alcohol withdrawal symptom assessment protocol, and administration of any benzodiazepine. Exclusion criteria were age < 18 years old, a known allergy to benzodiazepines, and pregnancy.
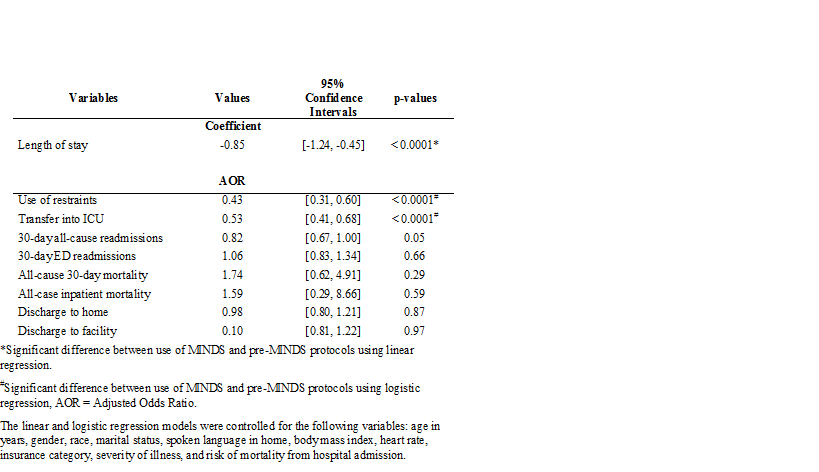
Results: MINDS patients were younger and fewer were married than Pre-MINDS patients and differences existed for race and insurance coverage (p < 0.001, Table 1). The MINDS group had a mean inpatient length of stay (LOS) that was 0.85 days significantly shorter than the Pre-MINDS group (p < 0.0001) when controlled for other variables (Table 2). MINDS patients were significantly less likely to require the use of restraints (AOR = 0.43, CI = 0.31, 0.60), and less likely to be transferred into the intensive care unit (ICU) (AOR = 0.53, CI = 0.41, 0.68). For patients transferred into the ICU, MINDS patients had a nonsignificant shorter LOS than Pre-MINDS patients. Both groups had similar outcomes for 30-day all-cause and emergency department readmissions, 30-day all-cause mortality, all-cause inpatient mortality, and discharge location.
Conclusions: For alcohol withdrawal patients, use of a novel symptom-based assessment tool and a single high dose diazepam-based treatment protocol significantly decreased LOS, use of restraints, and transfer into the ICU compared to use of multiple older protocols without adversely impacting readmissions and mortality. This standardized treatment approach can be safely used to improve patient outcomes.