Background: Resistance in learning (RIL) defines a set of attitudes or behaviors demonstrated by learners in an educational setting that result in decreased learning. Literature describes the etiology as multifactorial, including learning environment, characteristics of the learner, and teaching style. Hospitalists often use quality improvement methodology, such as PDSA cycles to improve the clinical care of inpatients. In conjunction with a team of academic hospitalists, we are using the same quality improvement methodology to address an educational problem within Phase I of medical school- resistance in learning. We are conducting a series of PDSA cycles to identify types of RIL during the Phase I pre-clinical years of medical school with the goal of implementing and evaluating an informed intervention within the curriculum to maximize both student academic success and the future benefit of patients. We hypothesize that reduction in RIL will contribute to higher USMLE Step 1 scores, higher satisfaction with the Phase 1 curriculum, and a decreased number of students who repeat courses.
Methods: A total of three PDSA cycles have been implemented. In Cycle 1 we conducted a student-faculty focus group using semi-structured questions. Focus group themes informed cycle 2 in which a survey was administered to 140 students. In Cycle 3 we implemented the “WISE” curriculum, designed to focus on Wellness, Integration, Step 1 preparation, and Education about learning. Motivation for learning will be surveyed throughout the new curriculum to evaluate change over time. Pre and post-curriculum USMLE Step 1 scores will be compared.
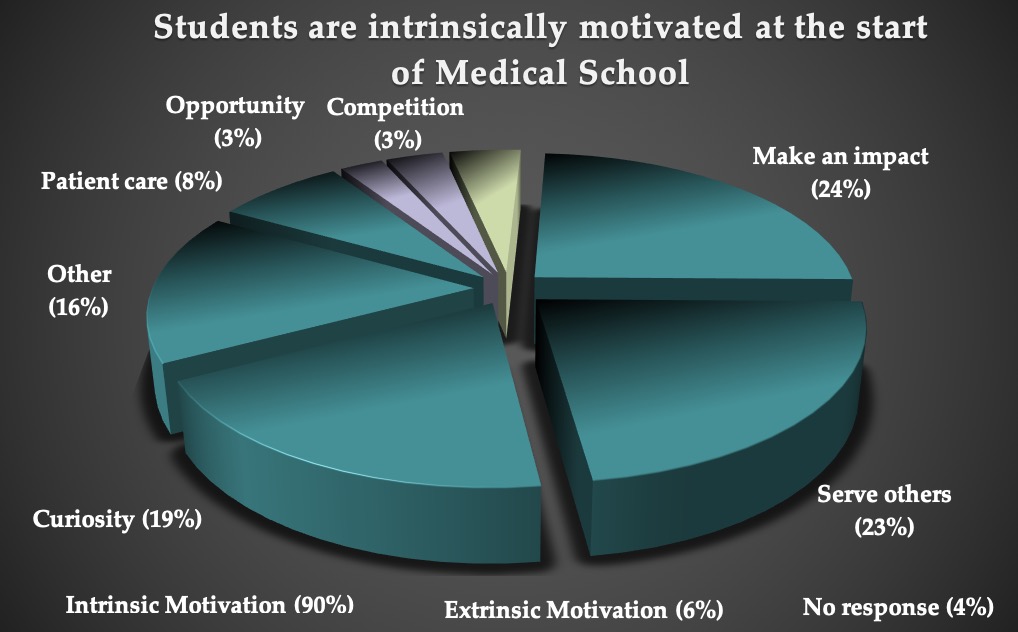
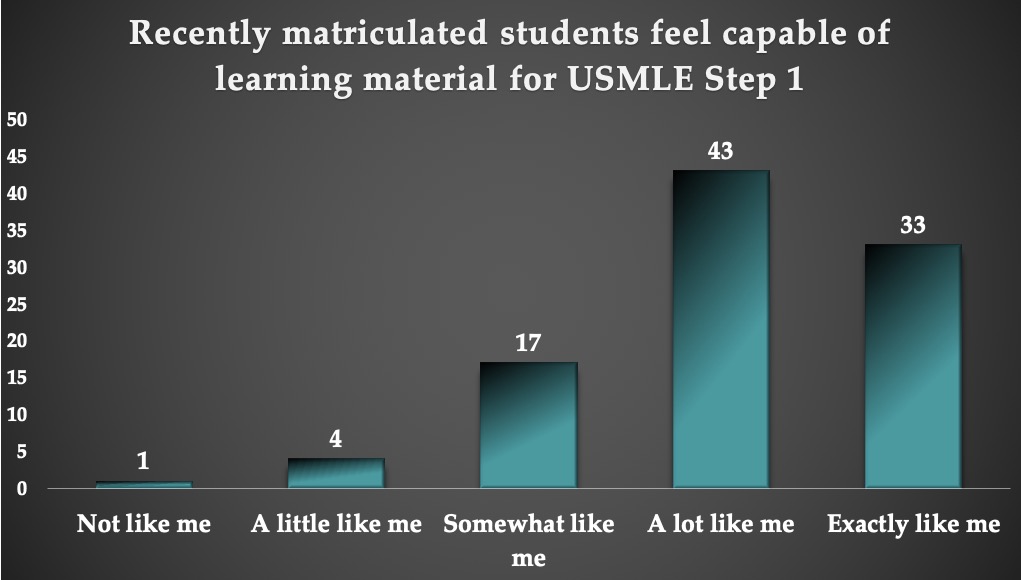
Results: Focus groups revealed the following themes: “Relevance,” “Motivation,” and “Alignment of curriculum with USMLE Step 1. Students surveyed on potential interventions asked for better alignment between the curriculum and USMLE Step 1, more consistency across the curriculum, and the opportunity to integrate concepts across systems early on and continuously throughout the curriculum. 90% of newly matriculated students cited an intrinsic motivation to enter medical school while 53% of second year students reported “finding relevance to USMLE Step 1” as their top reason for increased motivation to learn. 78% of students reported feeling highly capable of learning the content for USMLE Step 1 and 56% felt confident in their ability to achieve their academic goals. 93% of students prioritized “mastery goals”, yet 85% also endorsed “performance goals”.
Conclusions: Motivation to learn is increased by finding “relevance” in topics as they pertain to USMLE Step 1. Cycle 3 has revealed newly matriculated students maintain a strong sense of self efficacy in academic achievement. Students prioritize wanting to master content, although simultaneously have a desire to perform well. Students are intrinsically motivated at the start of medical school, citing making an impact and curiosity as their top motivations. However, as the curriculum progresses, motivation to learn is increased by making content more relevant to USMLE Step 1.