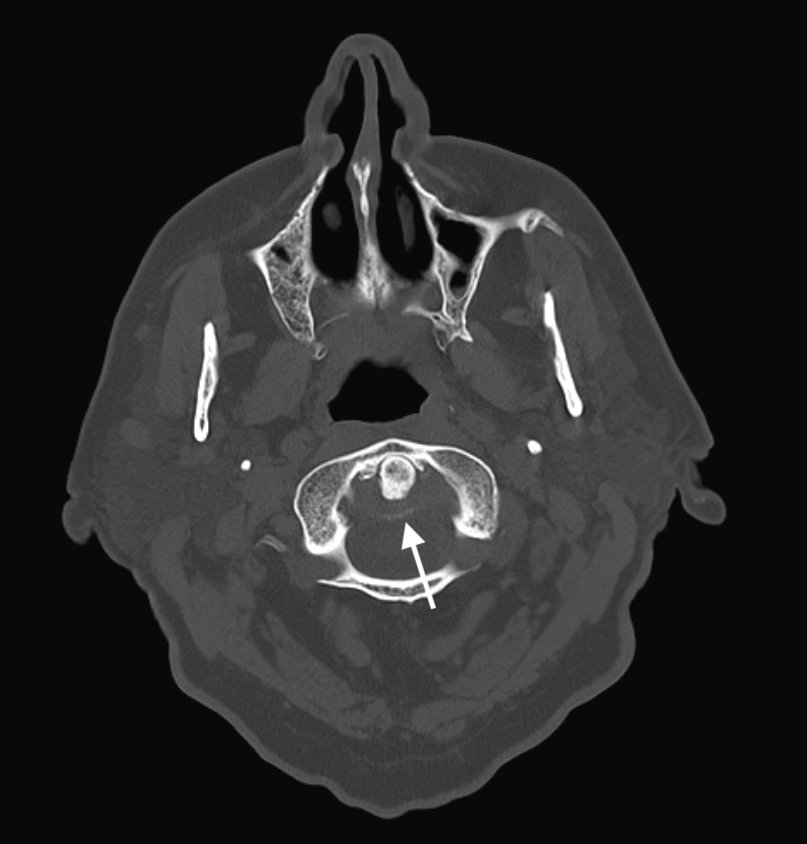
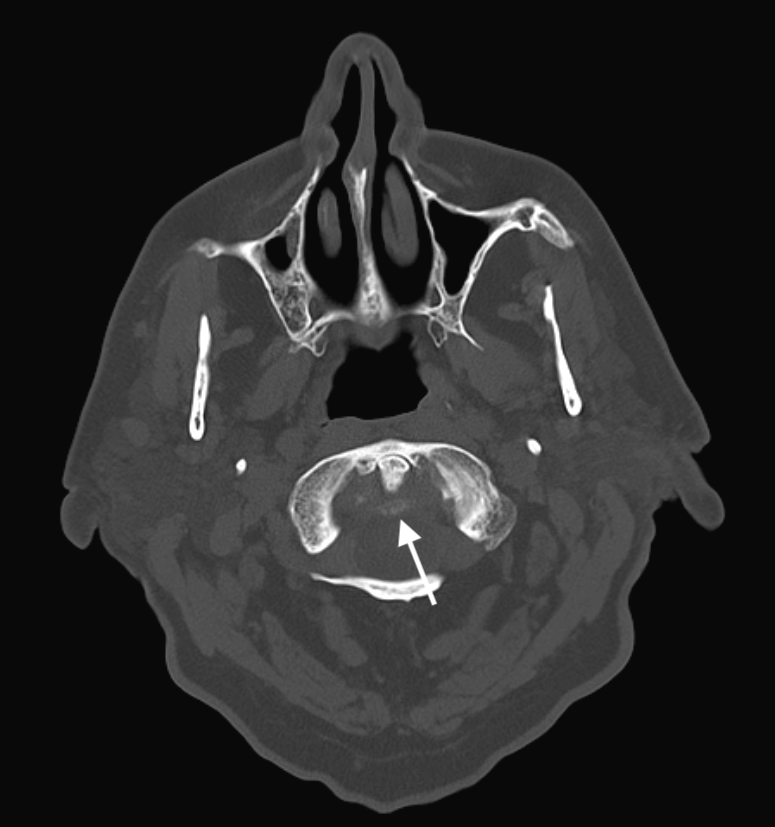
Case Presentation: An 89-year-old man with coronary artery disease, hypertension, and osteoarthritis presented with acute-onset severe posterior neck pain, with no viral prodrome. The patient reported experiencing generalized weakness and associated headache, but denied any fevers, chills, cough, myalgia, joint pain, ulcers or rashes. Additionally, he did not report any photophobia, phonophobia, changes in vision, or focal neurologic deficits.Upon examination, the patient was hypertensive (164/77 mmHg) and afebrile (36.9°C). Clinical findings included exquisite posterior neck point-tenderness that markedly reduced the patient’s neck range of motion. No abnormalities were noted on neurological exam. Laboratory results revealed an elevated ESR of 55 mm/h, CRP at 6.65 mg/L, and leukocytosis at 15.7 × 10^9/L. Uric acid and CPK were within normal limits. Head CT angiogram and brain MRI revealed no vascular anomalies, intracranial abnormalities, or evidence of infection. The patient declined a lumbar puncture and was started on empirical antibiotics for meningitis. On the second day of admission, prednisone was initiated for suspected myositis. This intervention resulted in a decline in CRP levels, but the patient’s pain did not ameliorate and worsened on the third day. Blood cultures were negative. In view of the absence of meningeal signs and constitutional symptoms, antibiotics were discontinued on day 3 without subsequent deterioration in the patient’s condition.On the fifth day, rheumatology was consulted for concerns of giant cell arteritis (GCA), given the patient’s ongoing headache and new report of jaw pain. Upon review of the imaging, the head CT revealed calcification of the periodontoid ligaments (figures 1a and 1b) with associated pannus at the C2 vertebra on MRI, consistent with crowned dens syndrome. The patient was treated with 3 daily doses of 100 mg of Anakinra and 40 mg of prednisone daily, resulting in a downtrend of his ESR and CRP. He was discharged on day 7 following significant improvement of his symptoms.
Discussion: Crowned Dens Syndrome (CDS), a rare presentation of pseudogout, involves calcium pyrophosphate crystals within the periodontoid ligaments of the C2 vertebra causing acute upper neck pain and stiffness, fever in the setting of elevated inflammatory markers, and potential neurological symptoms. Often misdiagnosed, it mimics conditions such as meningitis, GCA, or polymyalgia rheumatica. Diagnosis involves clinical suspicion, imaging studies, and exclusion of other causes. Imaging reveals pannus formation and calcification around the odontoid process. Mild cases may respond to NSAIDs or steroids, while severe cases as in our patient may require disease-modifying antirheumatic drugs (DMARDs) or IL-1R antagonists like Anakinra.
Conclusions: Prognosis for CDS is generally favorable with treatment, leading to significant improvement in symptoms. The rarity of the syndrome and potential for atypical presentations underscore the need for a comprehensive clinical evaluation and collaboration among medical specialties. Despite its infrequency, healthcare providers should be aware of CDS and radiologists should be familiar with subtle radiological findings associated with this condition. In our case, a more timely diagnosis would have been achieved had relevant findings been identified during the initial review of imaging. Rapid recognition and treatment of CDS are crucial for positive outcomes in affected patients.