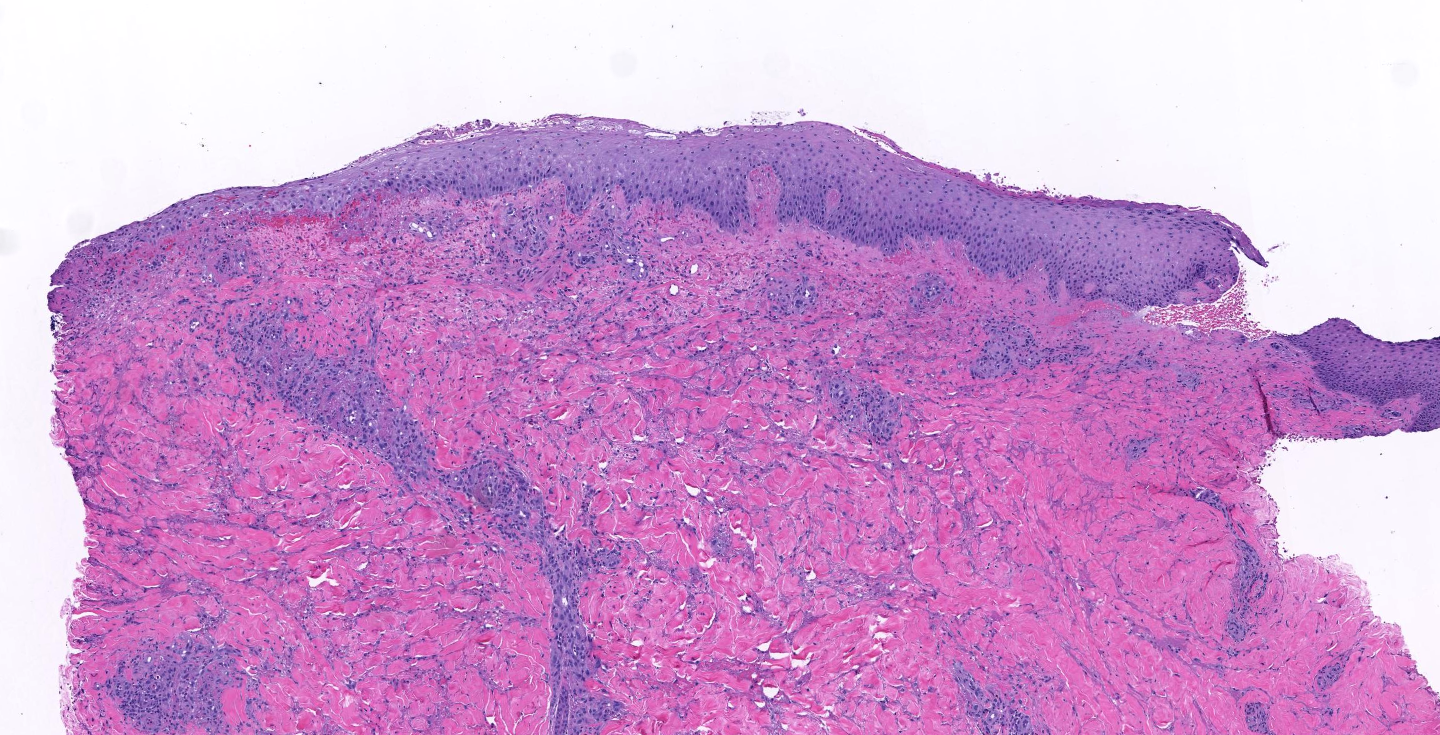
Case Presentation: A-28-year-old male with history of asthma and bipolar disorder presented to our hospital with a 10-day old, painful rash on bilateral lower extremities. History was significant for flea bites that occurred a day before the rash started. The rash started off as 3/10 petichae on both legs, but over 2 days it rapidly progressed to 10/10 painful petechial, blistering, crusted lesions. The rash had been treated with low dose oral clindamycin and topical hydrocortisone by his PCP for three days, which had resulted in mild improvement. The rash started progressing again immediately after he finished his course of steroids, prompting his presentation to the ED. On presentation to us, he had bilateral lower extremity edema. His lower extremity skin had a combination of lesions; purpura and bullae interspersed with scattered deep, necrotic craters with serous discharge (figure 1). All lesions were extremely tender to palpation. Review of systems was significant for dark urine, intermittent chills, and nausea.Lab work was initiated and was significant for leukocytosis and an elevated CRP and ESR. His comprehensive metabolic panel, C3/C4 levels, ANA and SPEP were unrevealing. A non-contrast CT scan of the lower extremity was non diagnostic, but suggested an infectious or inflammatory process. A working differential of vasculitis was made with special consideration for IGA vasculitis, small vessel vasculitis, and necrotizing vasculitis. Empiric treatment was started with systemic methyl-prednisone and broad spectrum antibiotics. He underwent a punch biopsy of the lesions. Pathology was significant for dermal necrosis, hemorrhage and ulceration (figure 2); findings consistent with leucocytoclastic vasculitis. Antibiotics were stopped and patient was discharged home on a short course of oral prednisone.
Discussion: – Leucocytoclastic vasculitis (LV) also called the hypersensitivity vasculitis, is a rare small-vessel inflammatory disease mediated by sub-endothelial deposition of immune complexes1-2 and subsequent invasion of the blood vessels by activated neutrophils.- This vasculitis is mostly Idiopathic, but certain medications (penicillin, cephalosporins, sulphonamides, phenytoin, allopurinol and many more1,2,4–6), and certain infections (hepatitis B and C, chronic bacteremia, HIV, and influenza7) are known associations.- In our patient a possible reaction to flea bite might have been the trigger- Management involves stopping the offending agent. First line therapy includes systemic glucocorticoids. Alternative therapy options include colchicine ans dapsone3, both of which suppress neutrophil function. Advanced immunosuppressive therapy is considered for refractory cases.
Conclusions: We report a rare case of severe leucocytoclastic vasculitis in response to flea bite. This disease can be best controlled by early identification and treatment. Complete history and physical with biopsy will help to identify the LV.