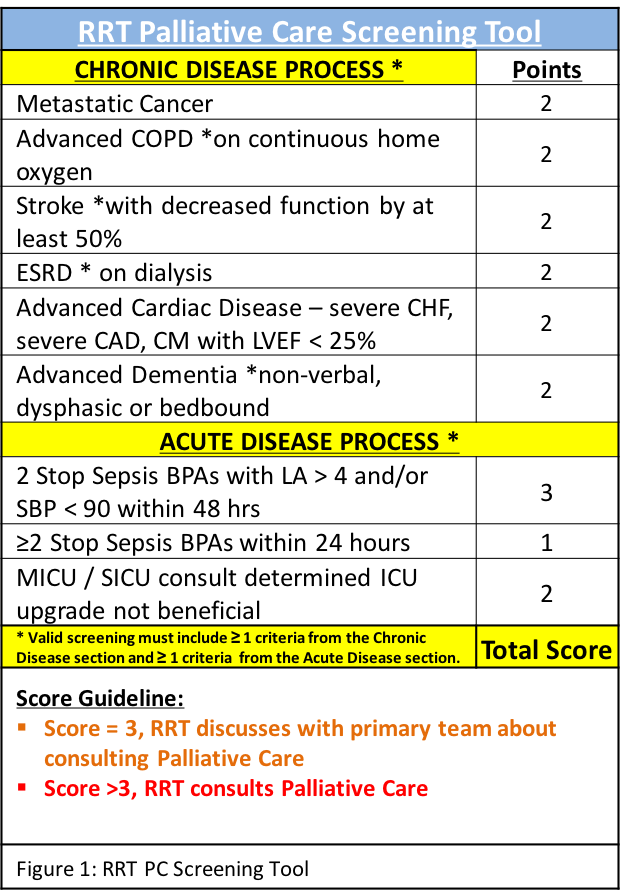
Background: Palliative care (PC) has been shown to be cost-effective and improve the quality of life for patients facing incurable and life-threatening illness. However, identifying patients benefiting from PC consultation remains a challenge in the inpatient setting. As part of a quality improvement initiative, we created a PC screening tool by adapting elements from existing outpatient tools to the inpatient setting. The 9-item PC tool aims to help guide PC consultation by identifying inpatients who would benefit from PC services. The tool has been incorporated into our hospital’s Rapid Response Team (RRT) work flow, where a PC score ≥ 4 triggers an automated consult to the palliative care service and a PC score of 3 prompts the RRT to recommend palliative care consultation to the primary team. The purpose of this project is to assess whether this PC tool accurately predicts patients who are at increased risk for mortality and would thus benefit from PC consultation.
Methods: We performed a retrospective chart review of patients who were screened using the PC tool. PC scores were only valid if they had at least one element from each of the chronic and acute portions of the tool (Figure 1). Assigned PC scores were either confirmed or corrected by trained study staff. PC scores were evaluated for their association with mortality (discharge status either listed as ‘Expired’ or ‘Hospice Care’) by chi-square for trend analysis. Corrected PC scores were used for analysis.
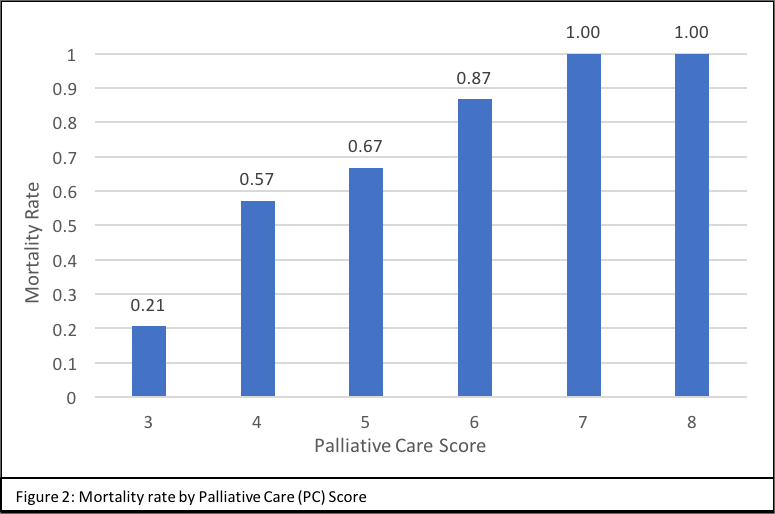
Results: Between April 2016 and May 2017, 161 patients were assigned PC scores ≥ 3 by the RRT screeners. Of these patients, 95 were retrospectively confirmed by the trained study staff to have met criteria of having at least one chronic and one acute item on the PC tool. The overall mortality for this group was 56.8%. Higher PC scores corresponded to increased mortality with mortality rates reaching 100% with PC scores >6 (chi-square for trend, p<0.001) (Figure 2).
Clinicians correctly assigned scores to 48 of 161 patients (29.8%) as determined by a trained study staff member.
Conclusions: The PC tool accurately identified non-ICU inpatients who were at increased risk for mortality. This analysis shows that using easily obtainable variables from patients’ medical records, physicians can reliably predict mortality risk and appropriately engage palliative care services. While the tool was predictive, screening clinicians incorrectly scored patients at a high rate (70.2%). Further investigation is required to determine how to increase clinician accuracy when utilizing this PC tool.