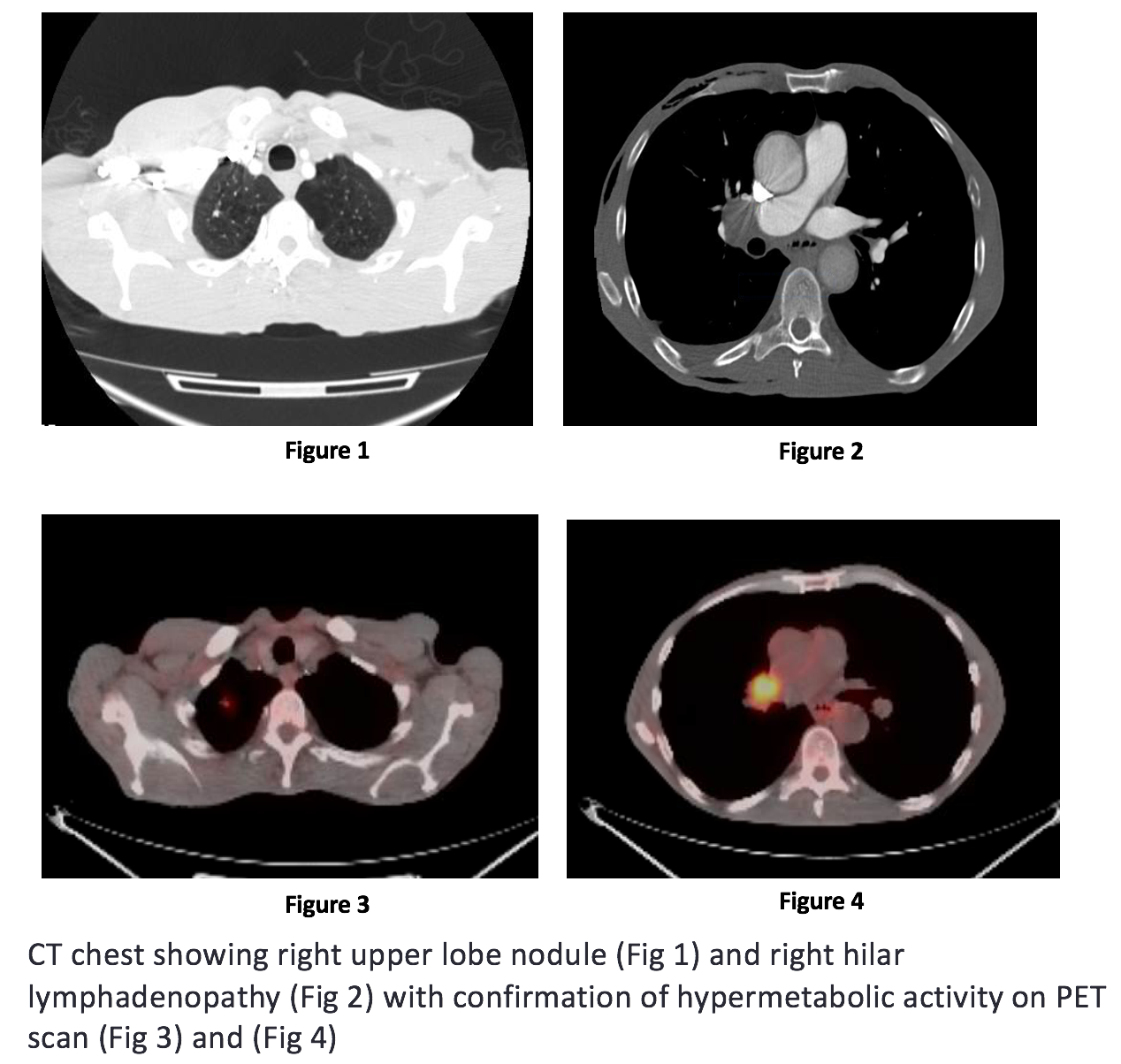
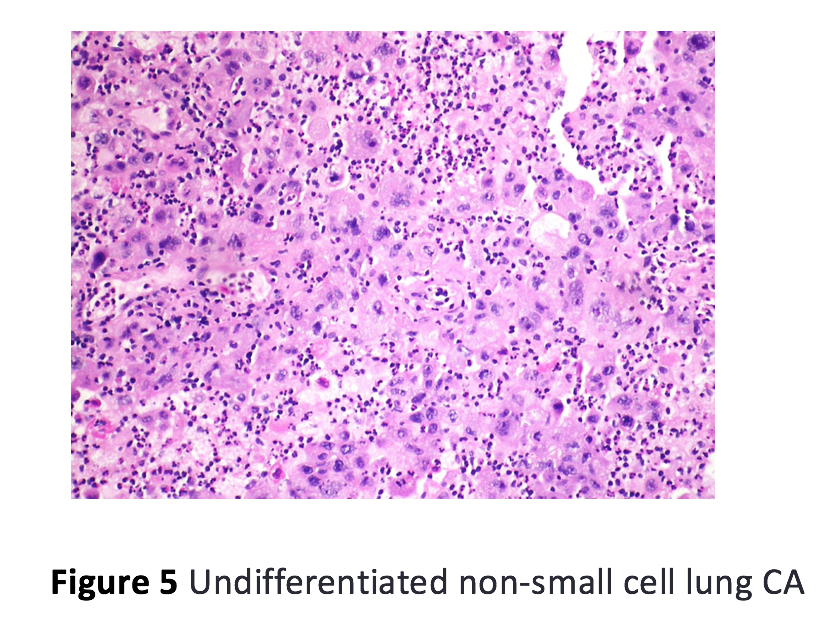
Case Presentation: A 61-year-old African American man with no significant medical history came to medical attention in December 2016 with severe post prandial bloating and vomiting for 2 months. On admission, vital signs and physical examination were unremarkable. The following laboratory tests were normal or negative: blood urea nitrogen, serum creatinine, bilirubin, alanine aminotransferase, aspartate aminotransferase, urinalysis, hemoglobin A1c, thyroid stimulating hormone, chest X-ray, electrocardiogram, computed tomography (CT) scan of the abdomen and upper gastrointestinal (GI) endoscopy. Further workup in the form of gastric emptying scan and small bowel follow through studies was consistent with generalized GI hypo-motility disorder of unclear etiology. CT scan of the chest showed a sub-centimeter spiculated nodule in right upper lobe of the lung with hypermetabolic activity seen on positron emission tomography (PET) scan consistent with malignancy. Nodule resection and biopsy showed poorly differentiated lung carcinoma. Serological testing was positive for neuronal nuclear antibodies (Anti-Hu, Anti-Ri) and cytoplasmic purkinje cell antibodies (Anti-YO). Overall clinical presentation was compatible with paraneoplastic GI hypo-motility disorder and patient was started on combined modality treatment with chemotherapy and radiation therapy for his lung cancer. Further modalities in the form of dietary modifications, pro-kinetic agents and psychological counselling were used for relief of his severe GI symptoms and clinical improvement was observed on follow-up visits.
Discussion: Paraneoplastic gastrointestinal syndromes rarely precede the actual detection of an overt cancer with gastroparesis being a very rare initial presentation. Likely pathogenesis is the destruction of neuronal ganglions with chronic inflammation of involved nerve fibers. Once the diagnosis is established, treatment is mainly supportive with removal of the antigen source by treating the tumor along with dietary modifications, pro-kinetic agents and psychological counseling for symptomatic relief. To increase the clinical awareness of this rare clinical entity, we are presenting this case of severe gastroparesis that was later proven to be associated with an overt poorly differentiated lung cancer.
Conclusions: After ruling out common etiologies first, unexplained gastroparesis should always prompt workup for an overt malignancy in the right clinical setting. Serological detection of anti-Hu antibodies is of clinical significance in the early diagnosis of paraneoplastic gastroparesis with a specificity and a sensitivity of 99% and 82% respectively.