Background: The patient-physician relationship is influenced by several factors including the environment of care. Given the increased use of telemedicine – catalyzed by the COVID-19 pandemic – understanding preferences for and comfort with telemedicine is important. This study aimed to explore patient preferences for various types of video visit background environments and their effects on the patient-physician relationship. Patient perceptions regarding elements of telemedicine visits were sought, as were sociodemographic factors that may influence access to and experience with telemedicine.
Methods: This cross-sectional survey study was conducted between February 2022 and October 2022. Participants included a random sample of adult patients who had completed an in-person or virtual outpatient visit within the prior year at either the University of Michigan or the VA Ann Arbor Healthcare System. Additional participants included registrants from a digital health research recruitment platform (UMHealthResearch.org). Surveys were distributed in paper and electronic formats and included photographs of a model physician in different environments. The primary outcome – preference for background environment – was calculated as the composite rating across 6 domains (how knowledgeable, trustworthy, caring, approachable, and professional the physician appeared, and how comfortable the physician made the respondent feel). Secondary outcomes included preferences for, comfort with, and influence of telemedicine as well as variation in preferences by respondent characteristics and institution.
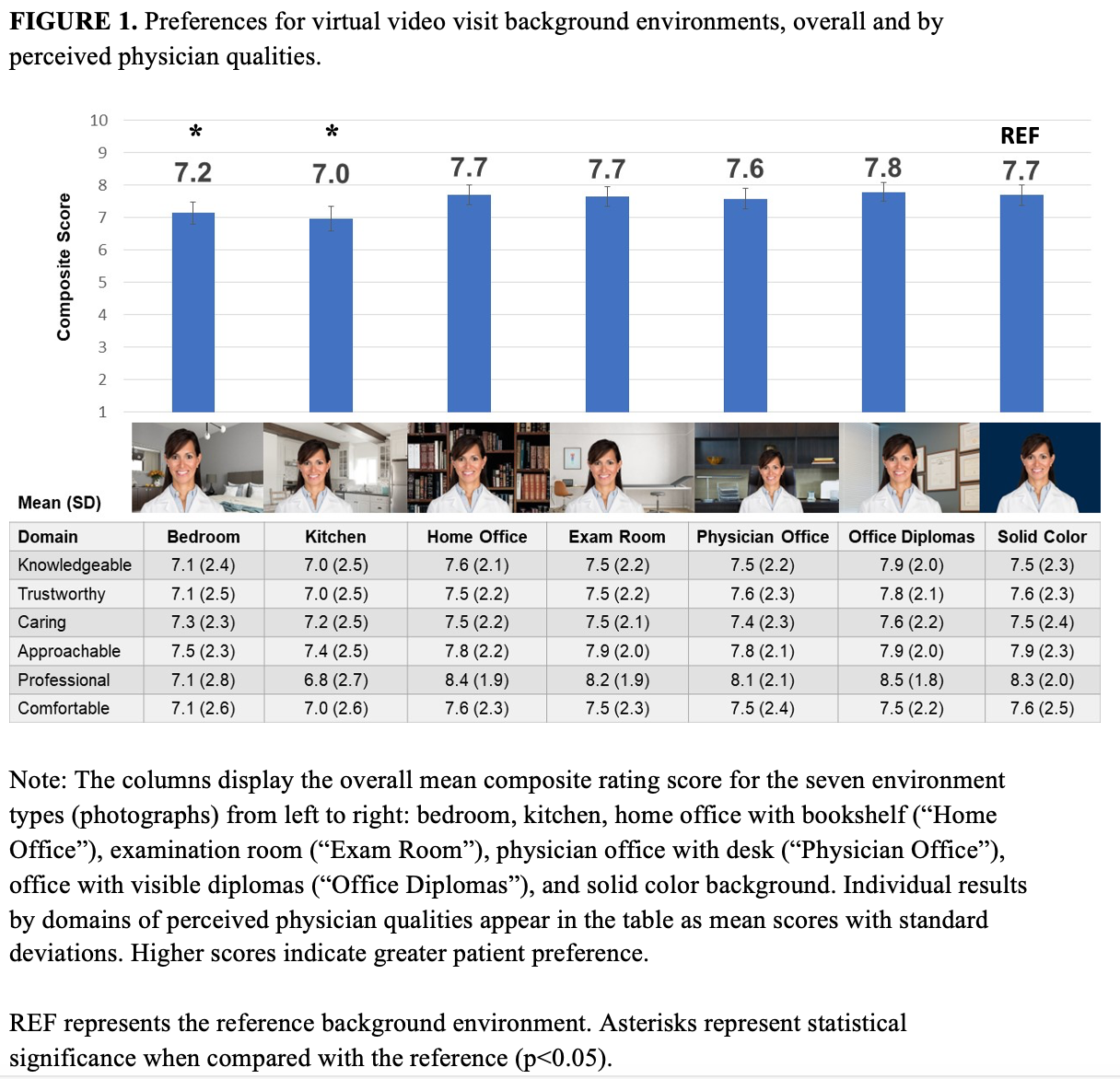
Results: A total of 1,213 patients returned surveys (response rates: 30% for University paper survey, 27% for Veteran paper survey, unknown for University electronic survey); 54.1% were 65 years or older; 53.3% were female. Respondents rated the physician office with visible diplomas as the most preferred background environment (mean composite score 7.8, Figure 1). This environment was also rated highest across 5 of 6 domains and scored highest for visits with established primary care (30.2%), new primary care (37.7%), established specialty (33.0%), and new specialty physicians (38.1%). Considering all physician types together and when compared with a solid color background (Figure 2), physician office and physician office with diplomas were significantly more preferred (p=0.007 and p< 0.001, respectively), whereas bedroom and kitchen backgrounds were significantly less preferred (p< 0.001 for both). There were no differences in preferences for home office and examination room when compared with the reference (p=0.27 and p=0.87, respectively). Most (77.4%) preferred in-person rather than telemedicine visits. Lack of broadband internet access and equipment, discomfort with video visits, and technological inability were disproportionately found among Veteran patients.
Conclusions: Patients have specific preferences regarding the background environment used during telemedicine video visits. Two-thirds of all participants preferred traditional office-based settings. Healthcare systems should prioritize performing telemedicine visits within a real or virtual office environment with visible diplomas, as this most resonates with patients. For telemedicine video modalities to be successful, all patients need equitable access to internet services, communication devices equipped with video capabilities, and education on their use.