Background: Sepsis affects over 19 million patients worldwide annually. While there was a reduction in in-hospital mortality for sepsis over the past two decades, the readmission rate among its survivors has increased. Sepsis is a leading cause of 30-day hospital readmission in the United States at 21.4%, compared to all-cause readmissions of 17%, and imposes an annual financial burden of $15–24 billion. Little is known about the role of SDOH in post-sepsis outcomes.
Methods: A questionnaire-based, multi-center, prospective pilot study was conducted to assess the feasibility of collecting current, accurate SDOH data and to explore SDOH association with unplanned 30-day hospital readmissions in hospitalized patients with sepsis. A cohort of adult patients discharged alive with a diagnosis of sepsis between February and June 2023 among three hospitals in North Carolina were included that had updated SDOH data collected on index sepsis admission to the hospital. Sepsis was defined based on the 2018 Center for Disease Control’s Adult Sepsis Event (ASE). We obtained SDOH data using a pre-built questionnaire available via the electronic health record (EHR). Patients were followed for 30 days post-discharge via EHR surveillance. We assessed the percentage of missing data for each category. The associations of SDOH with readmission were assessed using relative risk of readmission which estimated by modified Poisson regression with robust error variance. This research study received exempt status by the local IRB, and a waiver of consent was granted.
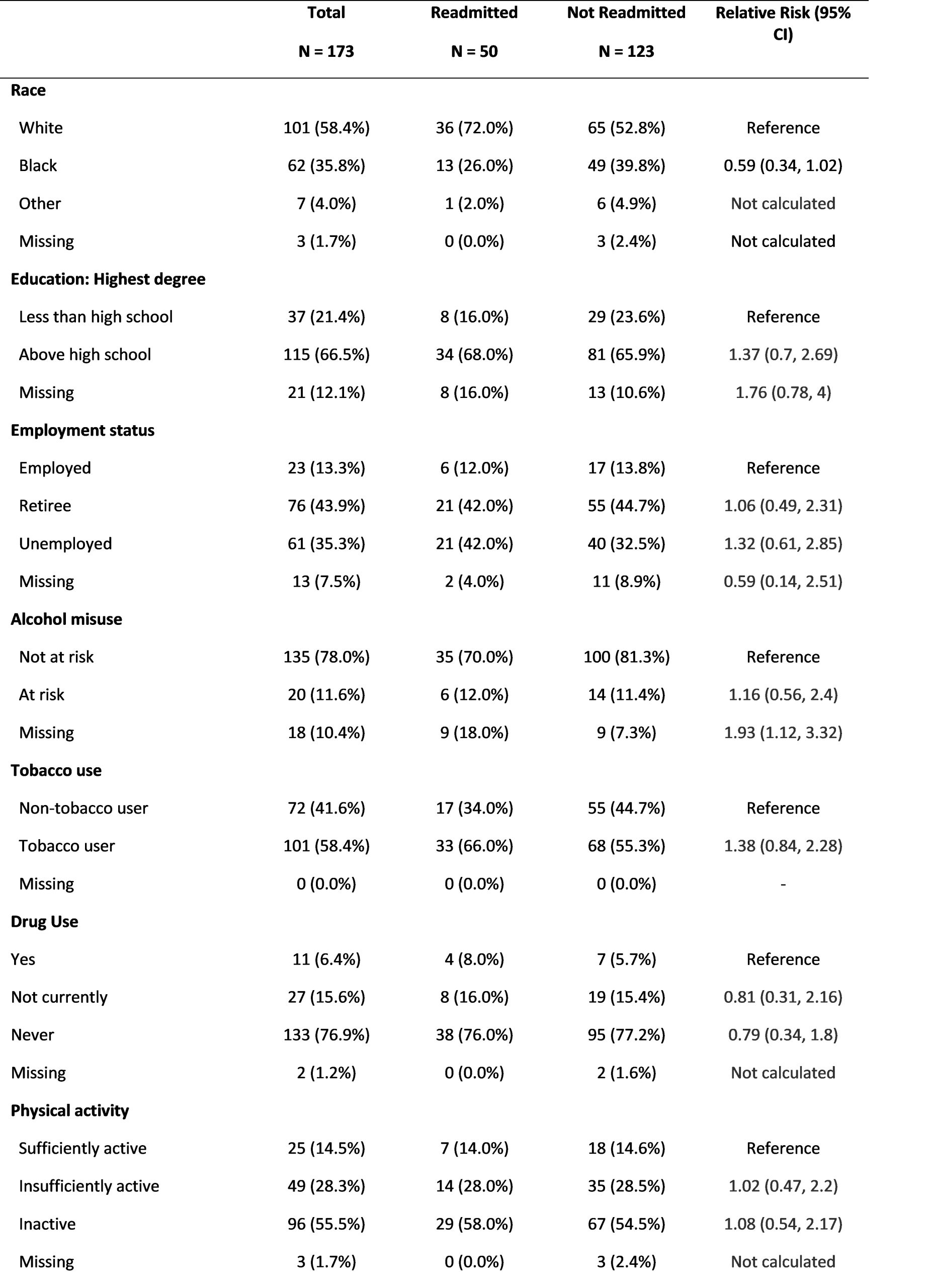
Results: Of 173 patients included, the mean age was 62.8 years old, with about 44% female. Over 87% had a primary care provider, and over 67% had Medicare. The most commonly seen source of sepsis was pneumonia (30.1%), followed by intra-abdominal (23.1%) and skin and soft tissue (20.2%). The median length of stay of the index hospitalization was 12 days (IQR: 7 to 23 days), and the median number of antimicrobial days was 13 (IQR: 8 to 28 days). The most common comorbidity was Diabetes (38.1%), followed by CHF (31.2%) and COPD (17.3%). Notably, 36.4% were immunosuppressed. The 30-day unplanned readmission and post-discharge mortality rates were 28.9% and 7.5%, respectively. Readmitted patients were found to have a higher mean Charlson comorbidity index (3.9 vs. 2.6) and higher mean EPIC readmission risk score at discharge (27.9 vs. 23.6) compared to non-readmitted patients. Fifteen SDOH were included with two having complete data and thirteen having 1.2% to 31.8% missing data. Numerically higher 30-day readmission rates were observed for some SDOH variables, such as white individuals, unemployed, and tobacco users.
Conclusions: This prospective evaluation of post-discharge sepsis outcomes is the first to evaluate a wide range of SDOH variables. The study provided valuable insights into the feasibility of collecting SDOH data and highlighting the encountered barriers and limitations. We demonstrated high readmission rates in the first 30 days after discharge that were most strongly dependent on chronic comorbidities and potentially SDOH variables, prompting a more in-depth exploration in the subsequent phase of the study with a larger cohort.