Background: Inpatient bedside whiteboards enhance patient-provider communication and satisfaction with care, but little is known about patients’ perspectives on the whiteboards. Our objectives were to understand patients’ views on the usability and design/content of these boards; and assess nursing views on current practice of whiteboard utilization, including barriers and suggestions to optimal use.
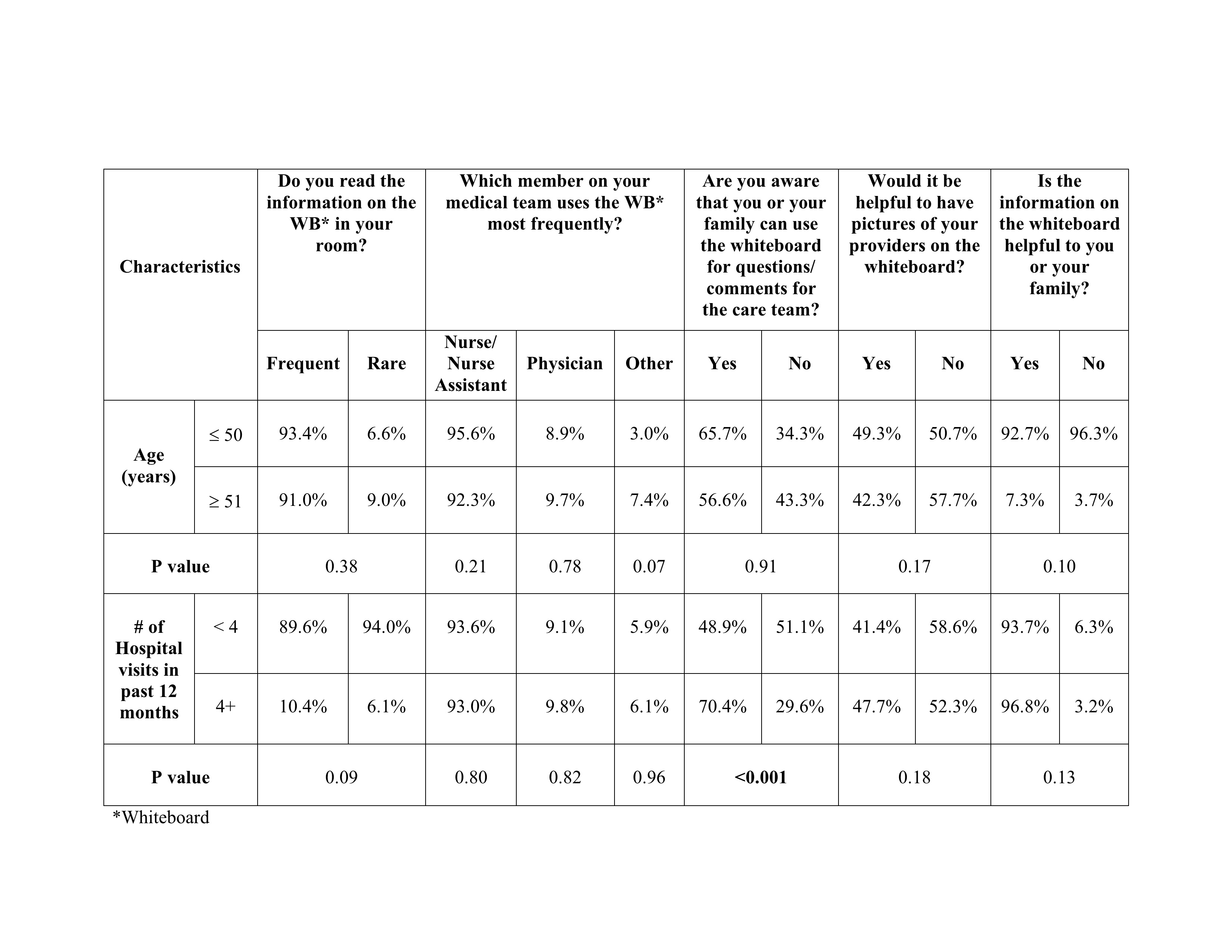
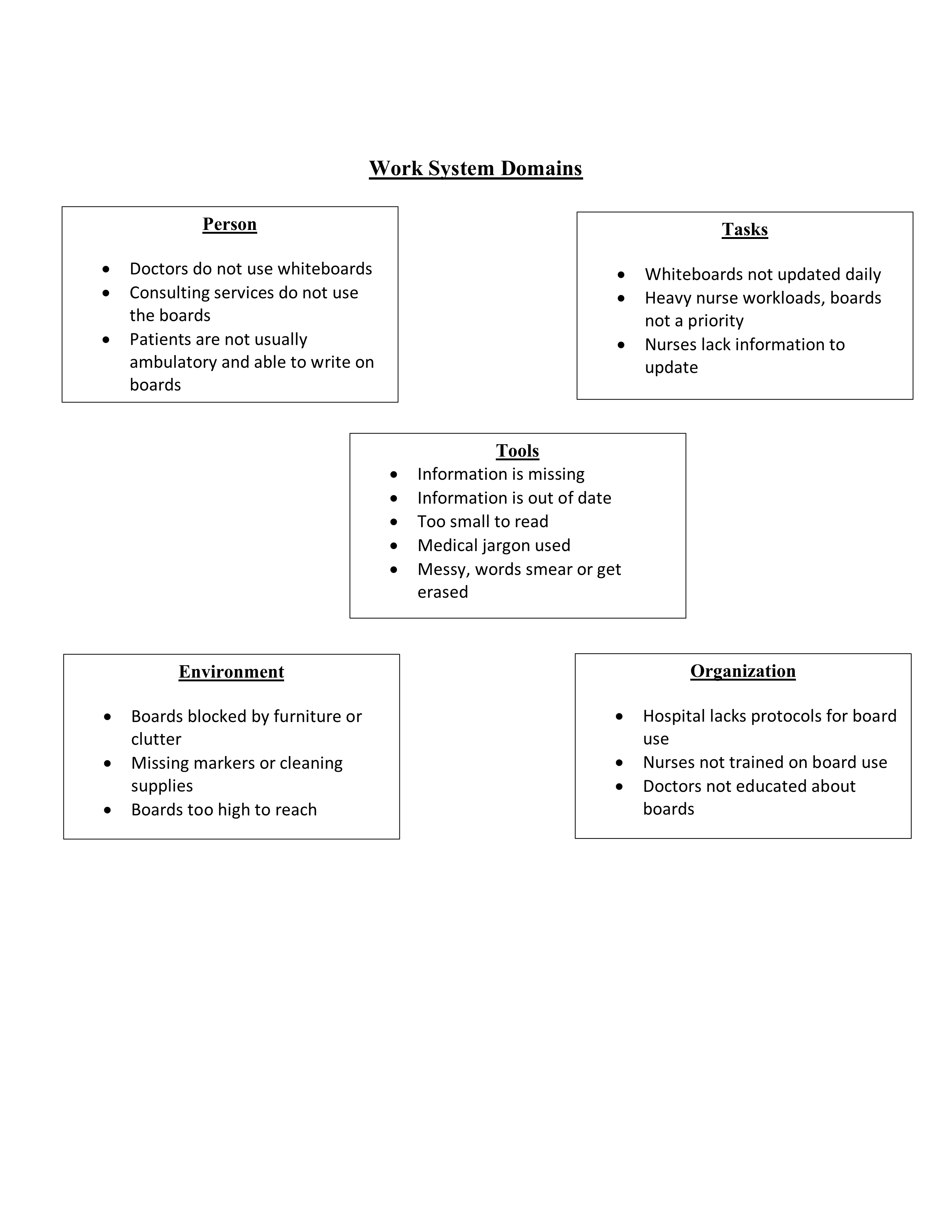
Methods: We conducted a mixed methods study of adult inpatients at a large academic center, along with nursing focus groups. Bedside surveys assessed patients’ views on whiteboards as follows: awareness and purpose of use; utilization by provider type; helpful information on the board; and utility of placing pictures of providers on the board. Data was dichotomized for bivariate comparison based on sex, age 50 or 51 years and average number of hospitalizations in past twelve months of < 4 or 4+. Nursing focus groups were conducted on two inpatient units using a semi-structured guide. Responses were organized into domains represented in the System Engineering Initiative for Patient Safety framework (person, tools, tasks, environment, and organization) to understand health system factors creating barriers to whiteboard use and potential opportunities for improvement.
Results: Of the 523 patients approached for interviews, 46 refused to participate and 39 were excluded, thus N= 438 patients. Respondents were more often males (55.05%), 51 years of age (68.7%) and admitted at least once in the past 12 months (50.6%). Over 90% of patients found the whiteboard easy to read and 91.8% read the whiteboard information frequently. The nurse/nurse assistant was identified as the most frequent user of the tool (93.3%) compared to physicians (9.4%). Name of care team members was most helpful (95%), followed by current date (87.3%), upcoming tests/procedures (80.3%) and goals of care (62.9%). 60% of the patients were aware that they could use the whiteboard for questions/comments for the providers and was statistically significant for patients with 4+ admissions in the past 12 months (p < 0.001). Only 55.4% respondents agreed that pictures of providers on the board would be helpful (Table 1.). Of 112 respondents, 19.6% suggested use of notepads/pens or electronic devices with inpatient portals (19.6%). Focus groups participants included 13 nurses, with varying roles from bedside nurses to supervisors. Overall, nurses felt responsible for maintaining the content on the boards. Reported barriers to use, included lack of access to updated clinical information (SEIPS domain for Task) and limited use by doctors and consulting services (SEIPs domain for Person) (Figure 1.). Suggestions to improve utilization included engagement of patients in adding information, questions or patient-centered goals to the whiteboards.
Conclusions: Our findings support that inpatient whiteboards are truly patient and family centered communication tools, and their full potential can be harnessed by simply orienting patient/family to their purpose, along with encouragement for daily use. Ideally, a whiteboard should be designed for the individual patient’s needs, however predefined templates work well for most patients. Future studies on integration of digital devices/portals to bedside whiteboards is needed to augment patient-provider information sharing.