Background: Clinical excellence is the mainstay of faculty development and advancement in academic hospital medicine groups (HMGs). Attaining clinical excellence relies heavily on feedback of current clinician skills. However, following completion of medical training, physicians and advanced practice providers (APPs) experience a gap in relevant and real-time feedback. A paucity of literature exists in academic HMGs in utilizing peer observation as a tool for faculty development. Current feedback models are primarily limited to learner evaluations and clinical case reviews, and rarely examine physician-APP feedback of each other in clinical practice. Yet, according to SHM’s 2018 State of Hospital Medicine Report, 88.9% of hospital medicine groups with 30 or more FTE employ APPs. An interdisciplinary team structure provides a potential robust opportunity for feedback among peers.
Purpose: We aimed to: 1) quantify peer feedback clinicians currently receive in our institution; 2) assess faculty opinions on a peer feedback process; 3) create an ongoing peer feedback platform to promote clinical excellence in our faculty.
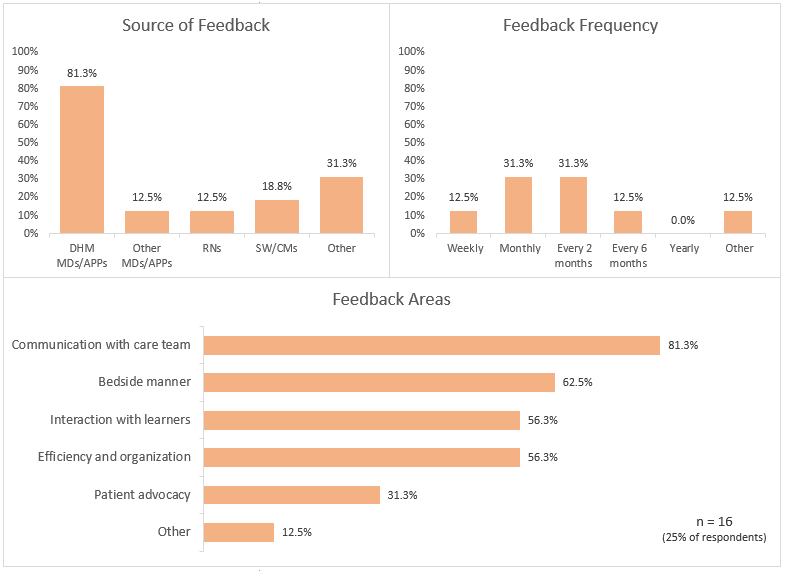
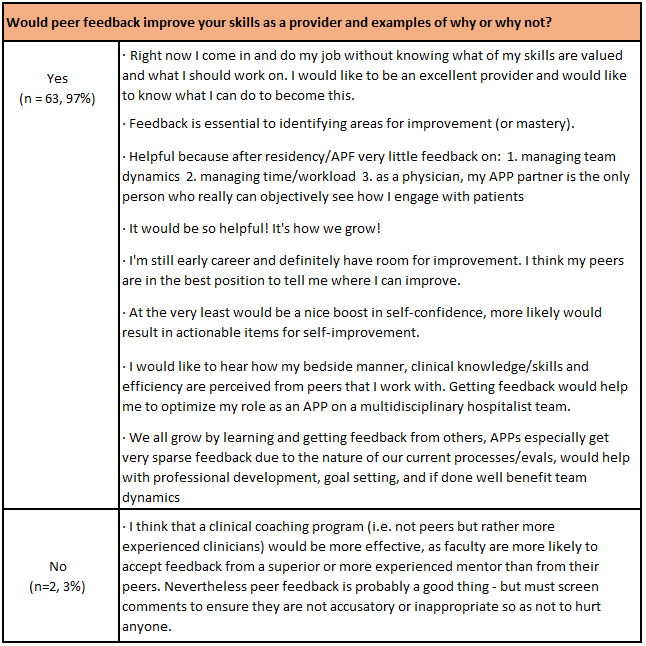
Description: A needs assessment was conducted through a survey of 101 academic hospitalists; 65 responses (42 physician, 23 APP) were received. When asked if they received clinical feedback, 75% (n=49) responded no while 25% (n=16) responded ‘yes’. Of the 16 who responded ‘yes’, details regarding the frequency, type of feedback, and who provided the feedback were ascertained (figure 1). Participants were asked if they felt peer feedback would improve their skills as a provider: 96.9% responded “yes.” Table 1 contains quotes detailing whether providers felt peer feedback would improve their skills. A formalized and simple 2-part peer feedback survey was created including the following questions: “What are three things this person does well?” and “What is one thing this person could improve upon?” This survey was sent to a pilot group consisting of 21 clinicians (11 physician, 10 APP) at the end of each clinical week of work for one month, asking them to provide real-time feedback to their physician or APP partner. At the end of the pilot, a debrief was performed with 13 participants who all reported this as a helpful, positive experience. Perceived benefits as reported by faculty included receiving positive feedback on their skills, understanding what could make the team work better next time, and having an opportunity to learn what went well and to learn how to continue growing. Perceived barriers included the feedback not being anonymous, potentially censoring the feedback a peer might otherwise give.
Conclusions: Despite a large gap in clinical feedback for academic hospitalists, a majority (96.9%) of hospitalist physicians and APPs at our institution express interest in receiving peer feedback. We created a formalized peer feedback platform to assist faculty development and advancement through highlighting individual strengths and opportunities for growth, thus facilitating clinical excellence. Additionally, this program may enhance the culture of physician-APP working relationships and advance divisional clinical expectations.