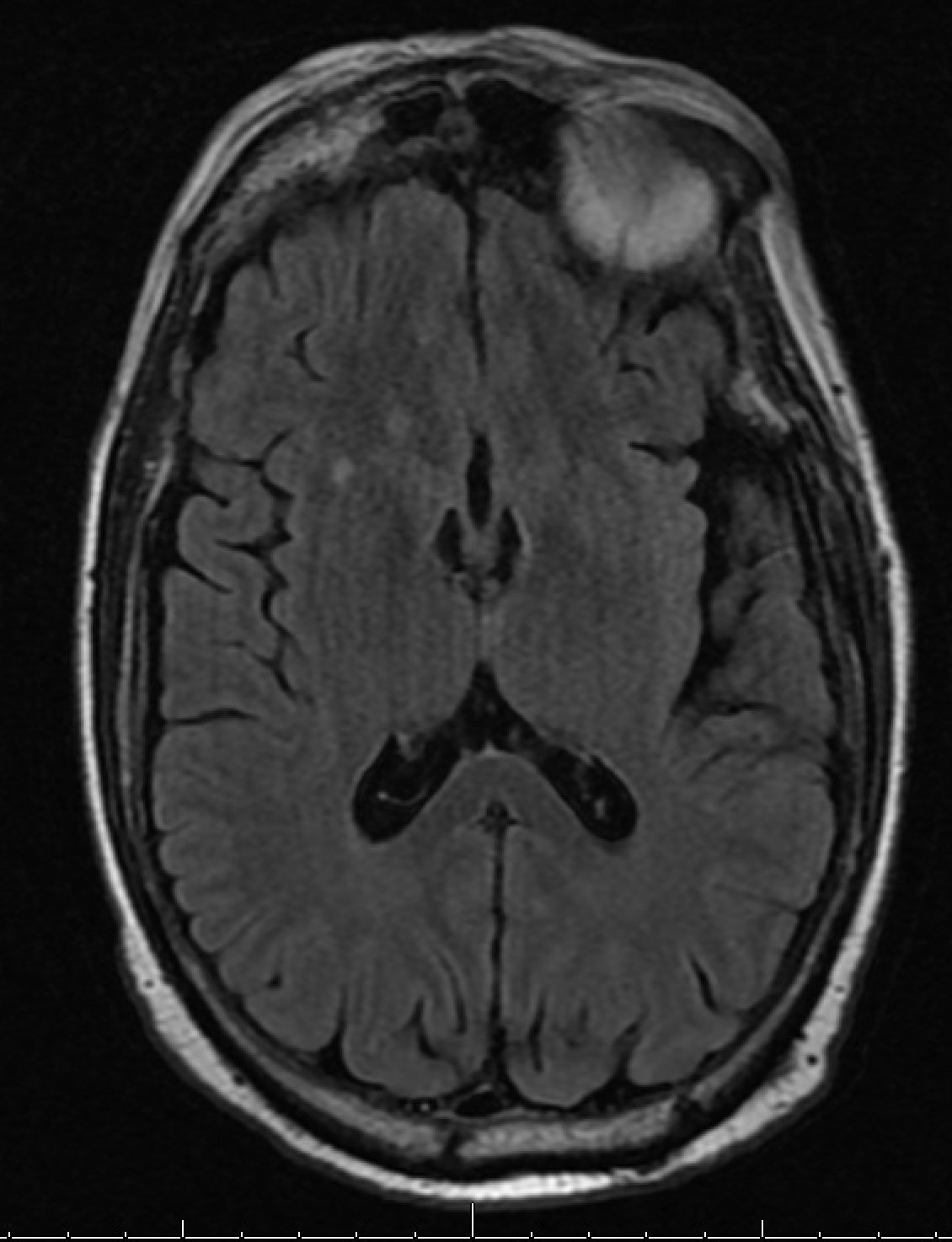
Case Presentation: A 55 yo male with past medical history significant for metastatic renal cell carcinoma with no clinical evidence of residual disease on maintenance pembrolizumab, alcohol abuse, hypertension, and chronic obstructive pulmonary disease, presented after a fall with unknown loss of consciousness and head trauma. His condition progressed to acute encephalopathy with sepsis, multiorgan failure and aspiration pneumonia. The patient developed delirium tremens due to alcohol withdrawal and required intubation secondary to respiratory distress. Toxic metabolic encephalopathy was initially felt to be due to chronic alcohol use vs paraneoplastic encephalopathy vs pembrolizumab related encephalitis. Lumbar puncture showed increased total protein and elevated lymphocytes. Cerebrospinal cytology was positive for atypical cells, but no clear evidence of metastatic disease. Cerebrospinal fluid paraneoplastic panel was negative. MRI and CT of the brain were non-diagnostic. Due to negative imaging and presence of inflammatory markers, encephalitis was attributed to pembrolizumab, which was promptly discontinued. The patient was treated with 5 days of intravenous immunoglobulin and steroids, with slow return to baseline mental status. A steroid taper was continued on discharge to inpatient rehabilitation.
Discussion: Immune checkpoint inhibitors (ICIs) such as pembrolizumab and nivolumab are increasingly being used for treatment of various diseases such as melanoma, non-small cell lung cancer, and renal cell carcinoma. As their mechanism of action is immune-activating, ICIs can trigger various immune-mediated toxicities. These include pneumonitis, colitis, nephritis, thyroiditis and encephalitis. Many of these toxicities are common and can be very severe. The exact mechanism is unclear, however studies point towards lymphocyte infiltration and resulting inflammation. Encephalitis is a rare complication seen with ICIs and can lead to significant long-term morbidity if not promptly recognized. Even less is known about the mechanism of encephalitis than in other toxicities from ICIs. The incidence of neurotoxicity in patients on ICI therapy is not well documented. A literature review showed that ICIs such as pembrolizumab have a neurotoxity incidence of about 6.1%. Diagnosis can be difficult due to the diverse range of symptoms that can be seen with encephalitis secondary to ICI use. Patients can present with both upper and lower motor neuron signs or with a constellation of neurological signs that do not fit one diagnosis. Imaging studies of the brain, cerebrospinal fluid studies and even electrical activity studies of the brain are often utilized to make this difficult diagnosis. Prompt discontinuation of the offending agent (ICI) and high-dose corticosteroids are the mainstay of treatment with severe ICI neurotoxicity.
Conclusions: The use of pembrolizumab and other ICIs has increased over the past several years. In conjunction with its use, adverse effects associated with these treatments has also increased. Encephalitis is a rare but possibly fatal complication of these medications. It is necessary to include ICI-induced toxicity in the differential for a patient with a history of malignancy currently or previously treated with ICI, who presents with altered mental status and markers of encephalitis or neurotoxicity. Prompt recognition, diagnosis and treatment with corticosteroids is of utmost importance to avoid long-term morbidity or possible mortality for these patients.