Background: Sitting at the bedside improves patients’ perception of their interactions with their physicians. Despite these data, prior work shows that medicine interns sit during only 9% of observed physician-patient interactions. We aimed to assess perceived importance of and barriers to sitting at the bedside among a group of internal medicine residents. These results have implications for ways to improve inpatient physician-patient communication and satisfaction.
Methods: We surveyed Internal Medicine housestaff at a large urban tertiary academic medical center anonymously using an electronic survey. The survey asked residents about their attitudes, practices, and perceived barriers around seated physician-patient interactions with inpatients.
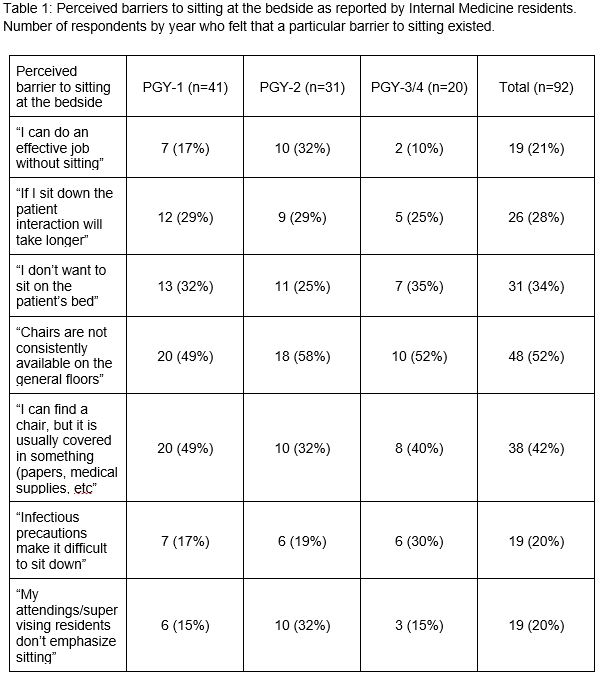
Results: We surveyed all 151 Internal Medicine residents at our institution, receiving 92 responses (61% response rate). Respondents represented residents from all post-graduate years. Residents perceived that they spent an average of 20% of their time in the hospital at the patient’s bedside. Seventy-three percent of residents also reported never or rarely feeling they spent enough time at the bedside. Residents felt that goals of care conversations (97% of responses), admission history and physical (71%), and new patient rounds with attendings (70%) were important times to be seated. Despite this, most residents reported using a standing posture (66%) rather than a sitting posture (32%) for performing admission histories. While some residents perceived that sitting would make the patient encounter longer, the absence of an appropriate chair in the patient room was reported as the dominant barrier to sitting (Table 1). Free text comments (n=16) on the survey suggested that residents also felt compelled to use the computer while talking to patients so they can be more efficient in writing their notes.
Conclusions: Across years of training, housestaff feel that sitting for communication is important at the time of admission and with significant patient updates, however they report standing more than sitting and that they do not spend enough time at the bedside. Significant perceived barriers include systemic issues of access to chairs and time demands on housestaff. Results of this survey suggest that deploying dedicated chairs for providers in the room may positively impact physician-patient communication during inpatient interactions.