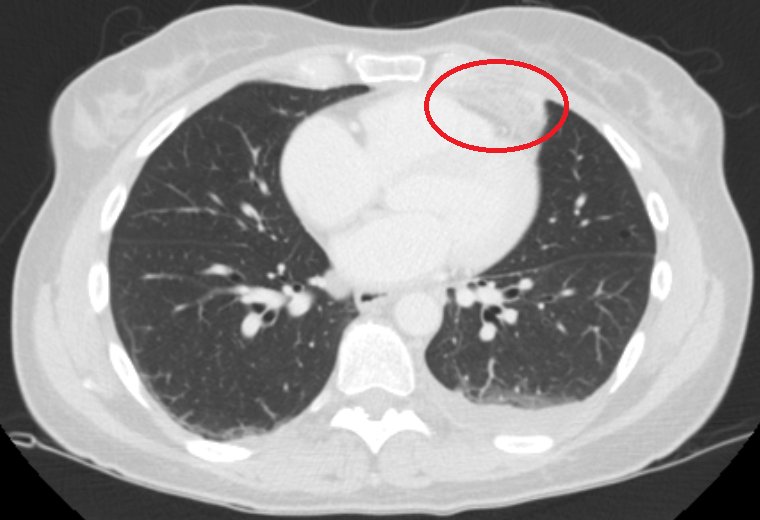
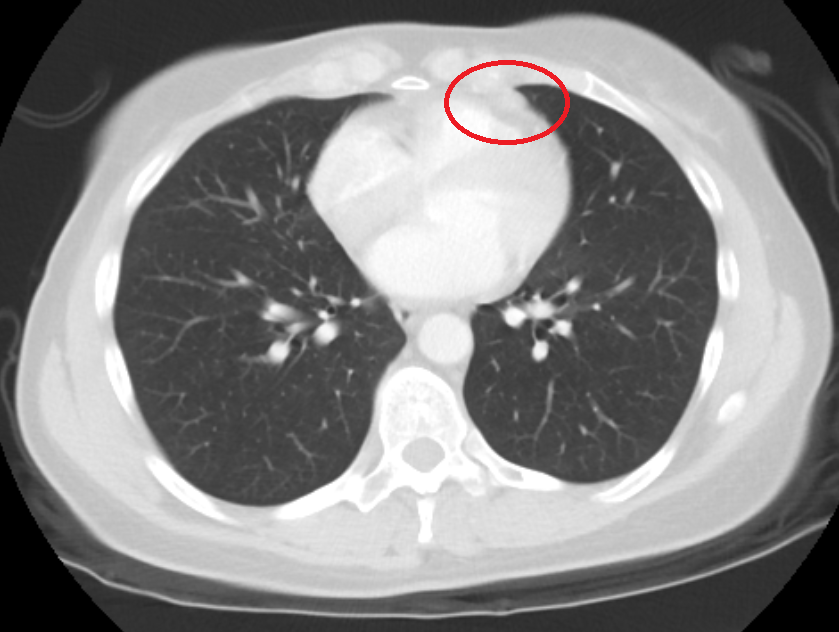
Case Presentation: We introduce you to a 57-year-old woman with a past medical history of one pack per day of smoking for 20 years, and a premature history of CAD in her father. The patient presented to the emergency department with severe, pleuritic chest pain that began 4 days prior to admission. The patient described the pain as sudden onset, 9/10 severity, occurring at rest with no association with exertion. On arrival, the patient was normotensive and stable. EKG showed sinus rhythm with frequent premature complexes, chest x-ray revealed no acute cardiopulmonary process, troponin markers and d-dimer were also negative. To rule out coronary artery disease, the patient underwent a CT Coronary Angiography (CTCA) which revealed no significant coronary artery disease or thoracic aorta dissection, however, it did show a heterogeneous lesion with fat densities along the anterior pericardium concerning for a neoplastic process, as well as groundglass opacities in the lingula, concerning for pneumonia. The patient was admitted to general medicine, and was started on ceftriaxone and azithromycin for community acquired pneumonia. Oncology was also consulted and a CT chest abdomen pelvis without contrast was done the following day to further characterize the mass and identify any other masses. SPEP / UPEP and tumor marker studies were also obtained. The scan revealed a pericardial fatty focus with intrinsic and surrounding soft tissue stranding measuring 2.2 x 3.0 x 3.2 cm, likely representing pericardial fat necrosis. The patient with discharged the next day on ibuprofen 400 mg TID for symptomatic management. The patient remained on NSAID therapy for three weeks. Approximately one month later, a repeat CT non-contrast chest was obtained which showed that the previously visualized heterogeneous pericardial fat lesion was nearly resolved, now measuring 1.2 x 0.5 cm. On follow up, the patient endorsed that her chest pain had significantly improved.
Discussion: Pericardial fat necrosis is a rare disease with an unknown incidence. It was first described in 1957 and review of literature reveals less than 30 case reports on it. It usually manifests as acute pleuritic chest pain, and workup for acute chest pathology such as acute coronary syndromes, pulmonary embolus are negative. The pathophysiology is not well understood, but several predisposing factors have been mentioned in the literature including trauma, ischemia due to torsion, obesity, and increased intrathoracic pressure leading to necrosis. CT is the imaging of choice as it allows for characterization of density measurements. The typical findings include an encapsulated, fat containing lesion with inflammatory changes such as dense strands and thickening of the pericardium. In the past, most cases were treated with surgical management. However, present day treatment is conservative with nonsteroidal anti-inflammatory drugs providing symptomatic relief. Follow-up imaging usually shows decrease in size.
Conclusions: Pericardial fat necrosis is a unique and infrequently encountered condition that often presents as an acute chest pain. It can mimic serious illnesses such as acute myocardial infarction, pulmonary embolism, and neoplasm, but has a rather benign and self-limiting course. It is important for physicians to be aware of this condition, as misdiagnosis can lead to unnecessary testing and further unwarranted work-up.