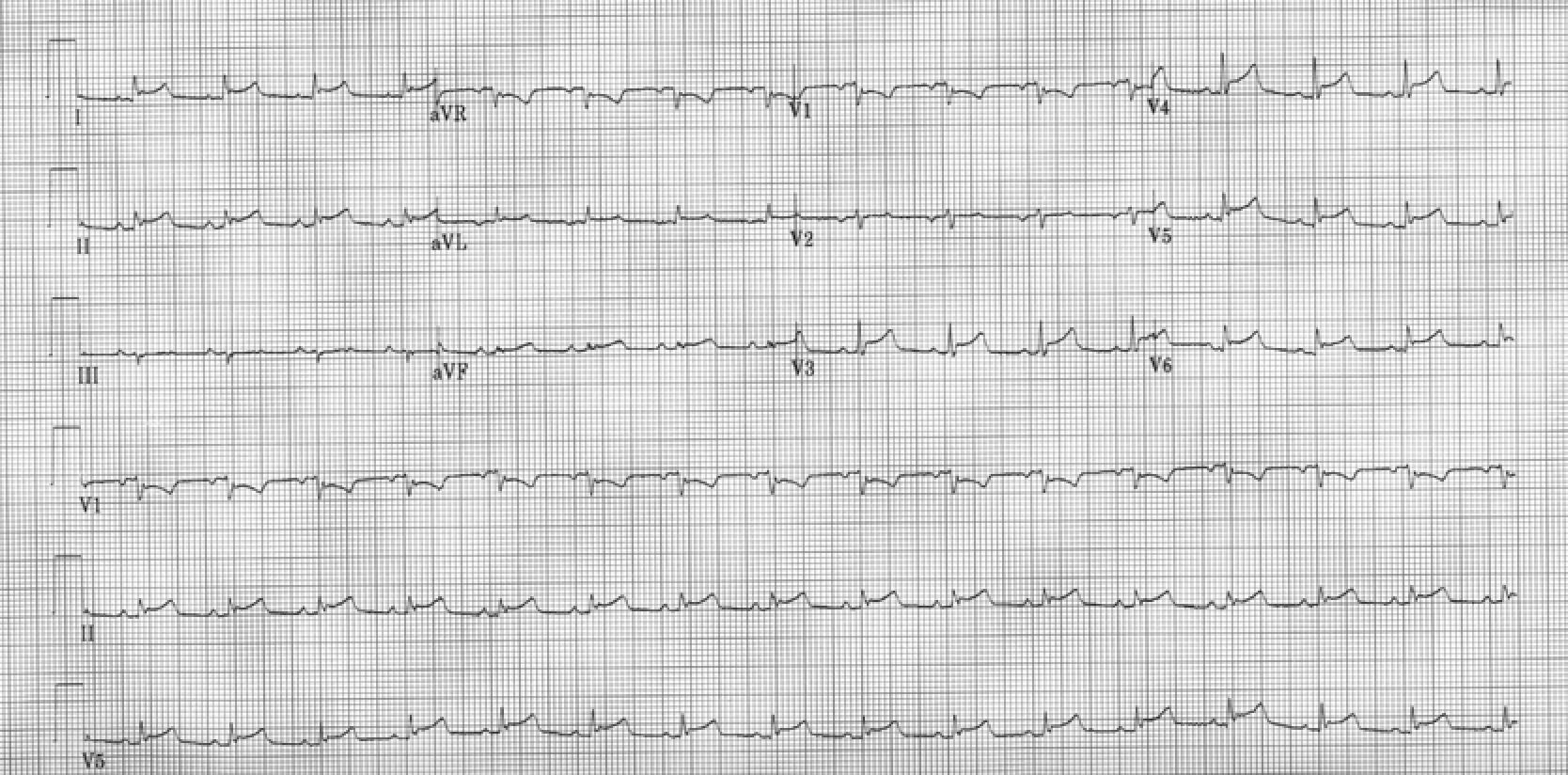
Case Presentation: A 68 year old caucasian female presented to the emergency department with 1 week of fever, chest pain, and dyspnea. On exam, she appeared cachectic and toxic . Her temperature was 101F, heart rate was 124/min, and she was in Atrial fibrillation. Her BP initially was 100/66, and respiratory rate was 25/min. Pulsus paradoxus was negative and jugular venous pressure was normal. EKG showed diffuse ST elevations suggestive of acute pericarditis. Labs showed 16.6K WBCs with neutrophilia, ESR 59, CRP 174, ALT 391, AST 698 and INR 2.19. Bedside trans thoracic echocardiogram showed a large pericardial effusion with no tamponade. Within 2 hours, heart rate rose to 170beats per minute , and her blood pressure began to decline. Her INR was reversed and emergent pericardiocentesis was performed for concern of progression to tamponade. 300 cc of serosanguinous fluid was drained, which showed 627 WBCs with neutrophilia. Gram stain of the pericardial fluid cultures grew gram positive cocci in clusters suggestive of staphylococcus aureus. Blood cultures grew methicillin sensitive staphylococcus aureus as well. IV Oxacillin was started and she was monitored in the Cardiac ICU. During her stay, she began developing worsening right sided pleural effusion. Thoracentesis showed 790 WBCs with 85% neutrophils, pH 7.44 and glucose 191.Post drainage imaging did not show a lung infiltrate. Pleural fluid cultures grew MSSA. A right sided chest tube was inserted, and TEE was negative for Endocarditis. Patient’s transaminases and INR improved post-pericardial drainage. She was discharged on IV Cefazolin for 6 weeks.
Discussion: The pericardium is anchored to its surrounding structures such as the manubrium sterni, the pleura and the vertebra via ligaments.Bacterial pericarditis in the post antibiotic era is rare and usually due to secondary infection or spread of infection from a contiguous focus via these ligaments. Mortality rate from bacterial pericarditis even with treatment varies from 40-75% and is due to tamponade, sepsis or constriction. It requires early recognition with echocardiogram and and prompt intervention with antibiotics and drainage. Thoracic surgery should be consulted as soon as possible to determine need for pericardial window, as fibrin deposition may occur making the percutaneous drainage incomplete.
Conclusions: When present, clinical suspicion for purulent pericarditis must be high and empiric broad spectrum antibiotics should be started , preferably a regimen that involves Vancomycin. Pericardial fluid should be checked for Gram stain and culture. Treatment for bacterial pericarditis typically is 4-6 weeks long. Pericardiectomy is rarely needed. .