Background: Vitamin K antagonists (VKA) remain widely used in the treatment of venous thromboembolism (VTE). During surgical interventions, the prevention of recurrent VTE must be weighed against the increased bleeding risk conferred by anticoagulation. There is a lack of strong evidence to guide the optimal periprocedural management of anticoagulation in patients with prior VTE, and in particular to identify those who would benefit from short-acting parenteral “bridging” therapy. We performed a systematic review to describe the risk of recurrent VTE and bleeding in patients with prior VTE, comparing periprocedural bridging with short-acting anticoagulants to VKA interruption without bridging.
Methods: We performed a systematic review of original articles in the Pubmed and EMBASE databases from inception through September, 2017 to identify studies reporting thrombotic or bleeding outcomes in patients on chronic VKA for secondary VTE prevention who required temporary interruption for an elective procedure. Two reviewers screened titles, abstracts, and appropriate full texts, and abstracted data on study design, patient characteristics, bridging strategies, and rates of recurrent VTE and major bleeding. We then qualitatively synthesized the outcomes of patients receiving periprocedural bridging and those who were not bridged.
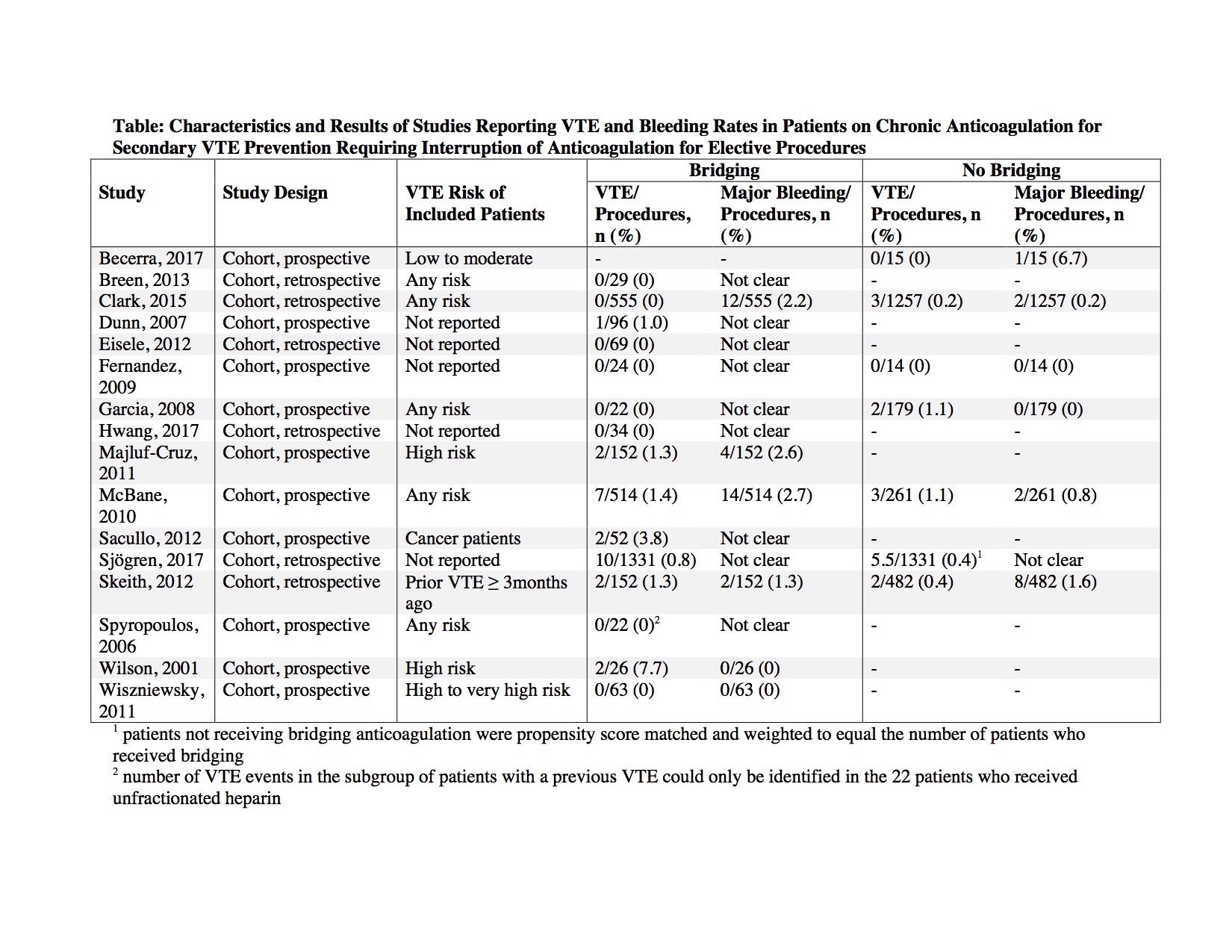
Results: Out of 2,476 articles screened, we identified 16 non-randomized studies and 0 randomized trials, for a total of 6,692 procedures. The estimated risk of VTE recurrence in included participants was reported in 11 of the 16 studies, ranging from low to very high. The incidence of VTE or major bleeding outcomes was directly compared across patients receiving periprocedural bridging and non-bridged patients in only 6 studies. Recurrent VTE events occurred in 26 of 3,141 (0.8%) procedures in bridged patients (30-day VTE risk ranging from 0 to 7.7%) and in 16 of 3,539 (0.5%) procedures in non-bridged patients (30-day VTE risk 0 to 1.1%, Table). Major bleeding rates were available in 6 studies and occurred in 32 of 1,462 (2.2%) procedures in bridged patients, and 13 of 2,208 (0.6%) procedures in non-bridged patients.
Conclusions: Our systematic review found only sparse observational data to guide the optimal periprocedural management of patients anticoagulated for VTE. Studies included heterogeneous populations and often lacked control groups. We found that the 30-day incidence of VTE recurrence during temporary anticoagulant interruption was low, even in patients who did not receive periprocedural bridging. High-quality randomized trials are needed to further clarify the role of short-acting anticoagulation during periods of VKA interruption.