Background: During a pre-intervention baseline survey period, only 38% of internal medicine inpatients with a do-not-resuscitate (DNR) order at time of hospital discharge and absent or discordant Portable Orders for Life-Sustaining Treatment (POLST) form at time of admission were discharged with a concordant POLST form.
Purpose: To improve documentation of end-of-life preferences in hospitalized adults admitted with an absent or discordant POLST form and who were discharged with a DNR order from the baseline of 38% to a goal of greater than 60% via a quality improvement initiative.
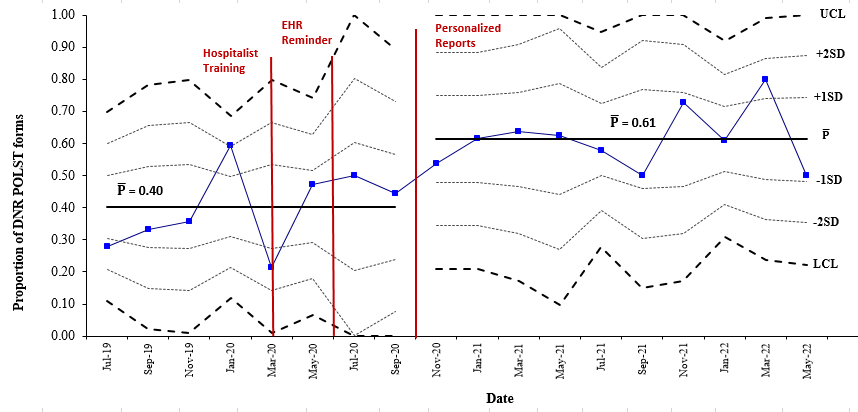
Description: Patient records were cross-referenced with the state’s POLST Registry for presence of a POLST form. Among patients with a missing or discordant POLST form at admission, we calculated the proportion for whom a concordant POLST form was completed by discharge. We tracked these data over time with control charts to detect performance shifts following several PDSA cycles that included education, an EMR alert, and quarterly individualized performance reports with blinded peer comparison emailed to internal medicine hospitalists. The proportion of DNR POLST forms completed at time of discharge population was 0.38 at baseline and increased to 0.61 after three PDSA cycles. A test of binomial proportions confirmed a statistically significant shift (p < 0.002) between March 2020 and May 2022.
Conclusions: A quality improvement initiative featuring personalized performance feedback improved POLST form completion rates in a target population of adults at elevated risk for readmission and death.