Background: Medication errors during hospital discharge can lead to adverse outcomes, medication-related readmissions, and increased healthcare costs [1,2]. Pharmacist-led medication reconciliation at discharge (PMRD) has emerged as a potential solution to mitigate poor outcomes and optimize medication safety [3-7]. The main objectives of this study were to determine the number of errors identified at discharge and characterize the patient harm prevented and associated financial impact.
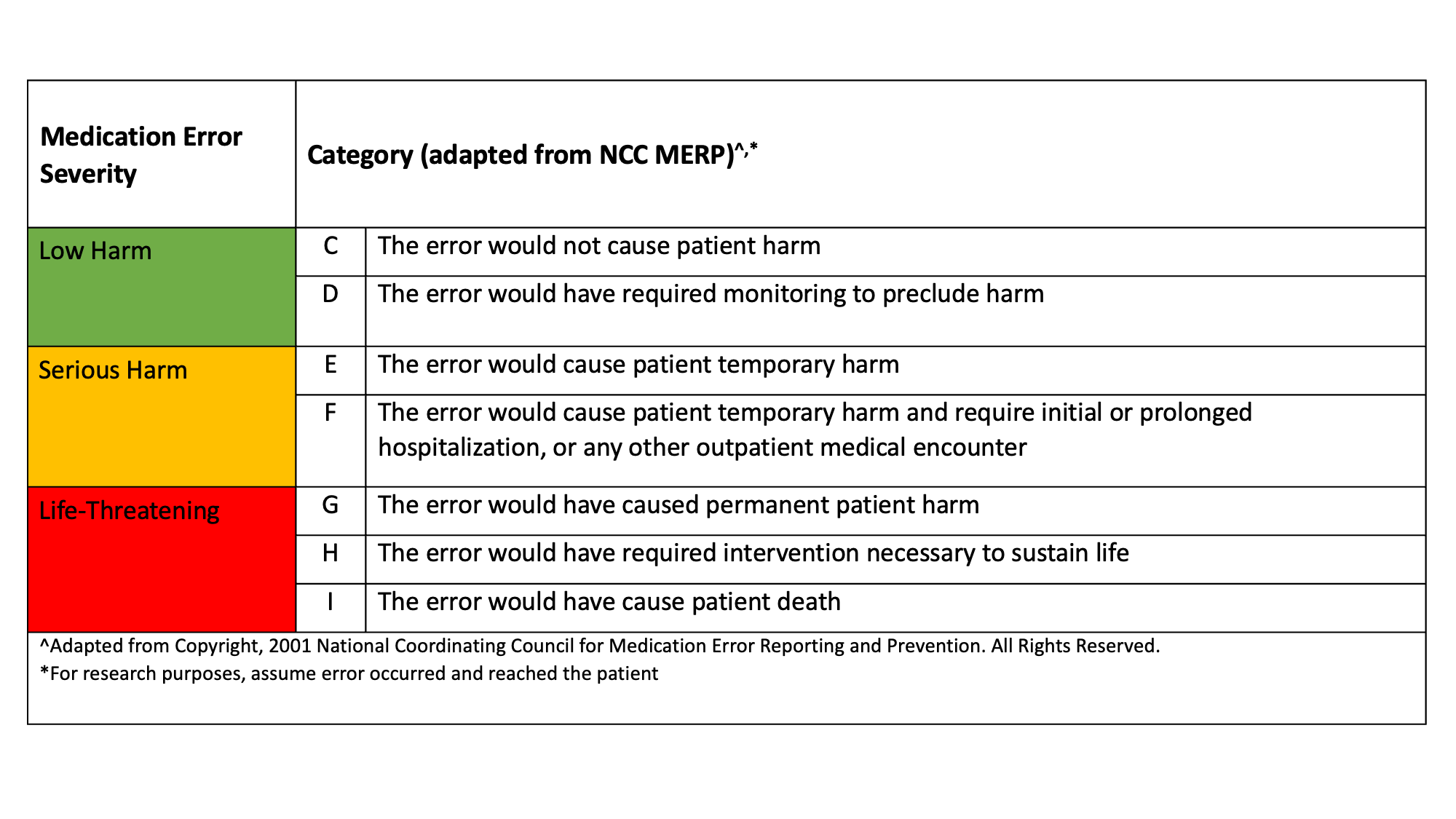
Methods: During a 4-week pilot prospective quality improvement study at a large academic center, a pharmacist on the adult internal medicine services performed discharge medication reconciliation. This included reviewing discharge orders for clinical appropriateness and discussing any discrepancies identified with the medical team. Number of errors identified at discharge were documented, categorized by type and adjudicated for severity of potential harm by a team of pharmacists with expertise in internal medicine and medication reconciliation. Error severity was classified based on a modified National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) Medication Error Index (Table 1) [8-9]. Two physicians were consulted to determine whether each error would have resulted in additional medical encounters and length of stay (no additional encounters, emergency care visit, or inpatient admission), with any discrepancies resolved by discussion with a third physician. Financial analysis included pharmacist labor for medication reconciliation and associated estimated cost savings from prevented emergency visits/hospital admissions.
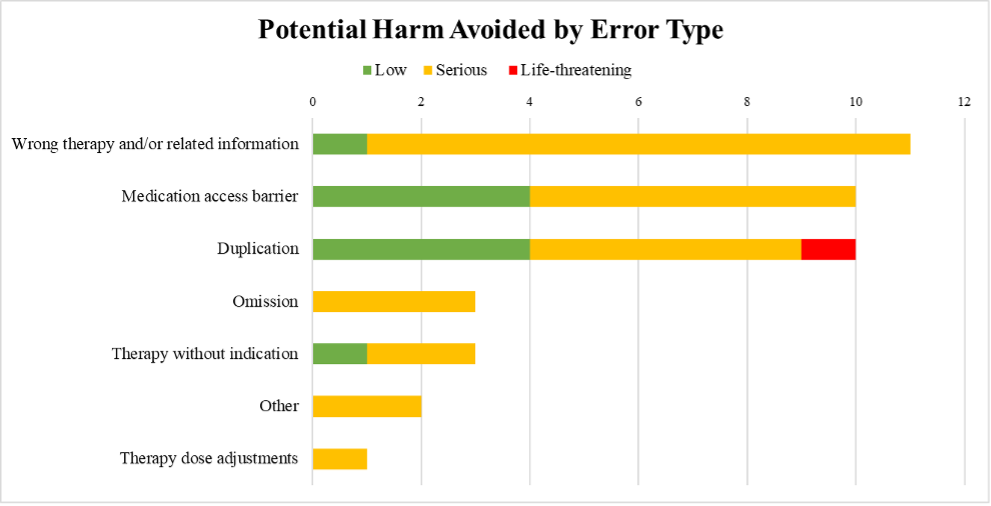
Results: A total of 31 patients were included in the analysis. Forty errors were identified by PMRD, with a mean of 1.3±1.9 errors per patient and 68% of patients having at least one error. The most common types of errors were duplication of therapy (25%) and medication access barriers at discharge (25%) (Figure 1). The severity of errors encountered included capacity for low (22.5%), serious (75%), and life-threatening harm (2.5%). Of the identified errors, 30% could lead to emergency visits, and 5% to hospital readmissions. The estimated total cost for these errors was $68,000. Pharmacist labor for reconciliation incurred a cost of $816. The total cost avoidance was $67,184 from the fourteen identified errors at discharge that could have resulted in additional emergency or inpatient visits.
Conclusions: Pharmacist-led medication reconciliation can prevent serious and life-threatening harm from reaching the patient, decrease cost from unnecessary health encounters, and stop the error from continuing across transitions of care. Following the significant outcomes of enhanced patient safety and cost reduction, this pilot study will be expanded hospital-wide to standardize pharmacist-led medication reconciliation at discharge.