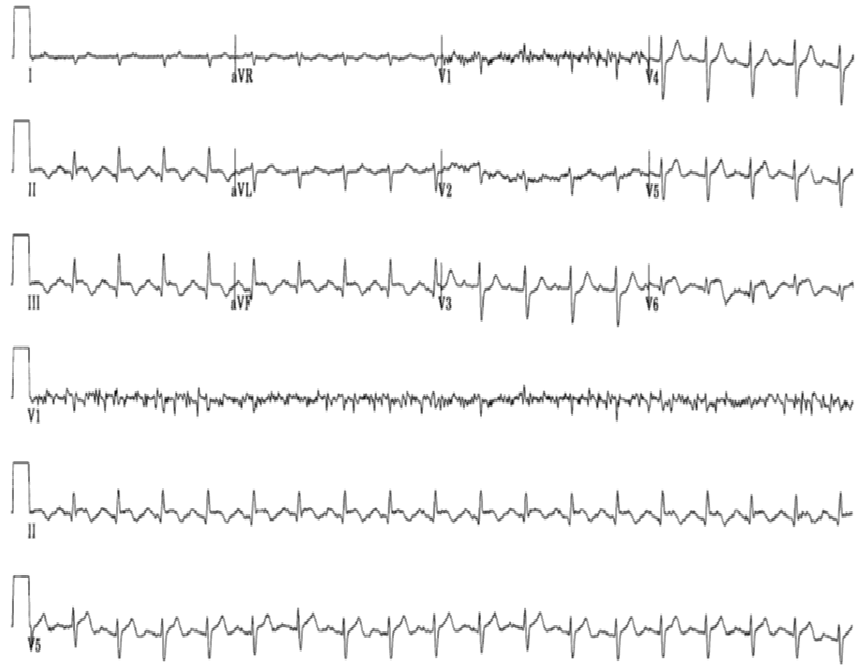
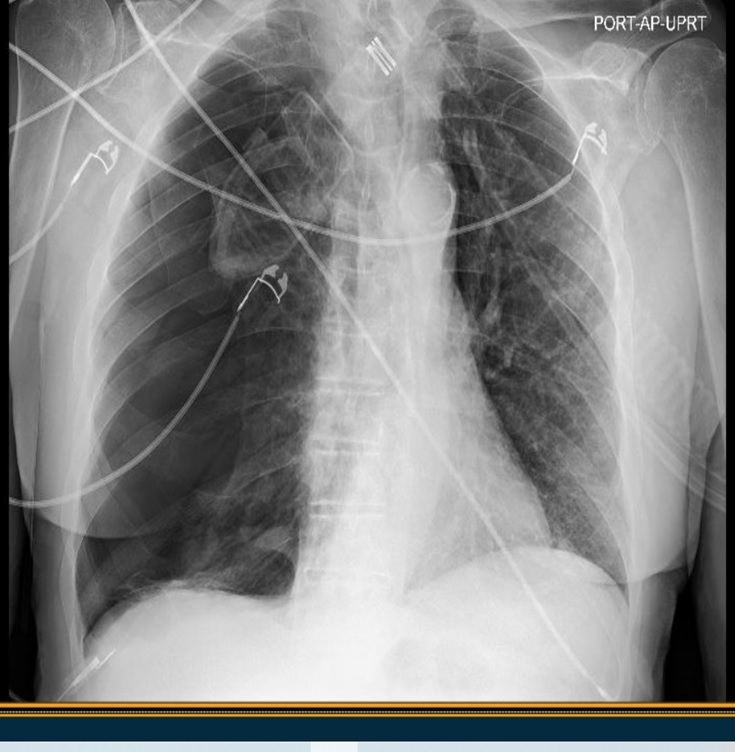
Case Presentation: 69-year-old female with a past medical history of coronary artery disease with prior percutaneous coronary intervention of the right coronary artery and left circumflex coronary artery, hypertension, hyperlipidemia, and COPD presented to an outside hospital with acute onset dyspnea and right-sided chest pain. ECG was obtained immediately upon arrival and was notable for ST-segment elevation in the inferior leads II, III, and aVF. Due to concern for acute myocardial infarction, STEMI protocol was activated, and preparations began to transfer the patient emergently to the nearest hospital with a catheterization laboratory. While waiting for the aeromedical transportation team to arrive, blood work and additional studies were completed. This included normal troponin I value of 0.011 ng/mL and repeat ECG, which was unchanged. Chest x-ray revealed a large, right-sided pneumothorax with leftward displacement of the mediastinum concerning for an impending tension pneumothorax. An emergent right-sided chest tube was placed, and post-procedure chest x-ray showed resolution of the pneumothorax. Emergent coronary angiography after arrival at the receiving hospital revealed open stents with no culprit lesions and otherwise unremarkable minor coronary artery disease. Five days later, the patient was discharged following removal of the chest tube. Etiology of the pneumothorax was thought to be due to the severe coughing bouts that the patient had shortly before the onset of chest pain.
Discussion: Pneumothoraces can cause ECG changes [1]. With right-sided pneumothoraces, in addition to ST-segment changes, several other changes can occur, including right- and left-axis shifts, QRS complex changes such as incomplete right bundle branch block, and increases and decreases in the amplitudes of the QRS complexes in the precordial leads [2]. Proposed mechanisms for these ECG changes include cardiac rotation and displacement from the pneumothorax, ventricular dilatation, and an insulation effect on electrical signals secondary to air that is present between the heart and the chest wall [3]. Although the patient in this case had a normal troponin I value, cardiac enzyme elevations can occur with pneumothoraces [4]. Treatment frequently consists of a chest tube, which may be preceded by needle decompression under emergent circumstances. Following treatment of the pneumothorax by removal of the air in the thoracic cavity, ECG changes can resolve [5].
Conclusions: This case illustrates a unique cause of ST-segment elevation from a pneumothorax rather than the more common myocardial ischemia. When confronted with a patient having chest pain, regardless of the findings of the initial ECG, hospitalists should also obtain baseline chest imaging as part of the initial work-up for chest pain. Even routine tests such as a portable chest x-ray or bedside point-of-care ultrasound can quickly provide additional critical and important information that can help to rule out emergent and life-threatening pathologies that may not be detected by an ECG alone. In this case, if the pneumothorax in this patient had not been diagnosed and treated with a chest tube prior to air transport, it could have progressed to a tension pneumothorax during transit. Some of the facts related to this case may have been changed to protect the identity of the patient.