Background: In 2016, around 94% of healthcare facility managers used locum tenens physicians in the previous 12 months. One-quarter of them were locum hospitalists, making hospitalists as the second most common service in demand for locum physicians. There are no prospective studies comparing the care of locum to non-locum hospitalists.
Methods: We conducted a classical prospective cohort study. Consecutive patients were recruited dynamically between 2/25/2019 -4/30/2019. Patients included were ≥18 years admitted to IM services for any reason. Excluded patients who did not consent and patients admitted to academic services. We collected the following data: age, sex, ethnicity, assistance at home, food security most the year, residence prior to admission, type of insurance, admission diagnosis (16 categories) and comorbidities (17 categories). In-hospital mortality, 30-day all-cause readmission, and 30-day mortality were outcomes of interest. Propensity score by inverse probability of treatment weighting. Subsequently, we fitted weighted multiple cox proportional hazard for readmission and 30-day mortality to compare locum and non-locum services. Baseline characteristics were compared using parametric and non-parametric analysis. Diagnostics were used to assess propensity score model and multiple regression models. We matched patients seen solely by locum (n=49) to patients seen solely by non-locum (n=296) and subsequently obtained average treatment on the treated. To account for cross over, complete cohort (n=747) was standardized to obtain “locum-percentage” exposure. Locum-percentage was calculated by diving locum physician-days by the sum or locum-days and non-locum-days for each patient. Locum-percentage ranged from 0% when the patient was entirely cared by non-locum physicians up to 100% when the patient was entirely treated by a locum hospitalist. Locum percentage was used as an independent variable to fit regression models to estimate the average treatment effect.
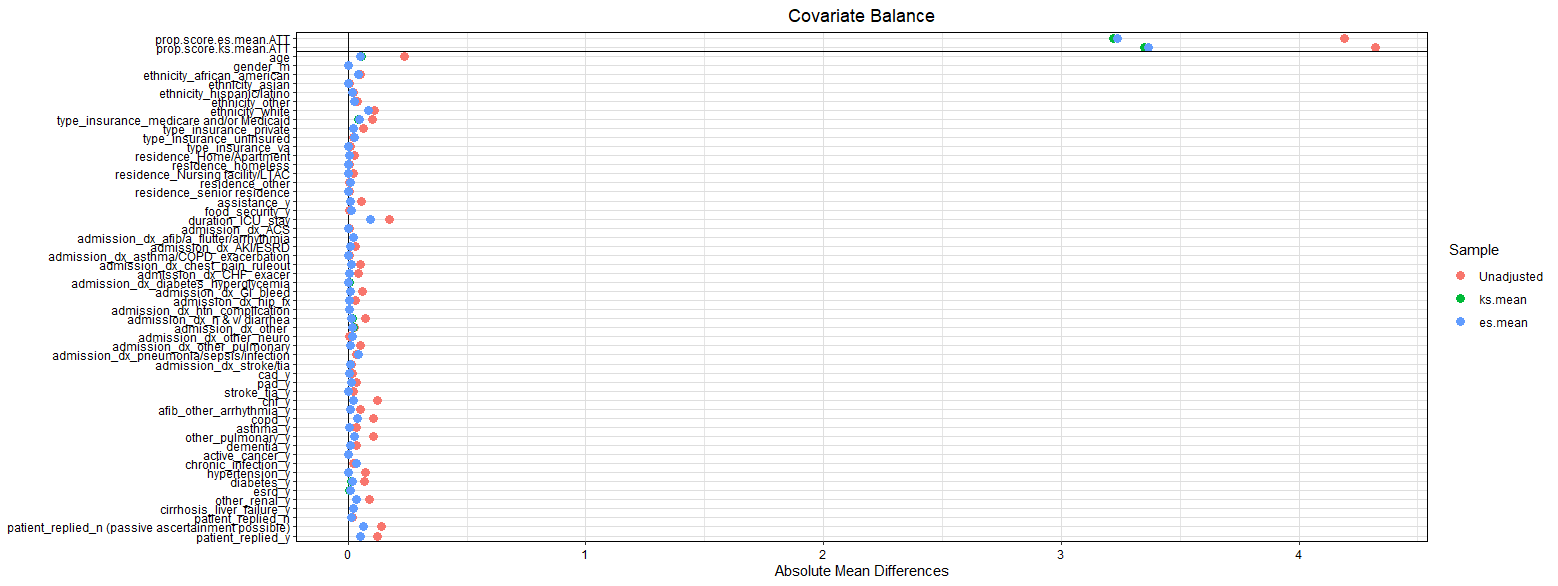
Results: A total of 747 patients were admitted in the study period. The mean age was 60.5 ± 19 years and females were 52%. Baseline characteristics were well balanced with standardized biases less <0.1 post propensity matching. Using the adjusted data, there was no difference in inpatient mortality (p-value= 1). There was no difference in 30-day readmission or 30-day mortality on log-rank analysis (p-value= 0.66, p-value= 0.28). No difference was seen in readmission (HR=0.4, p-value=0.5) on multiple cox proportional hazard regression. Similarly, no difference in readmission (HR=1.5, p-value=0.2) or mortality (HR=0.5, p-value=0.4) was seen using locum percentage as exposure.
Conclusions: There was no difference in in-hospital mortality, 30-day readmission or 30-day mortality between locum and non-locum hospitalist services.