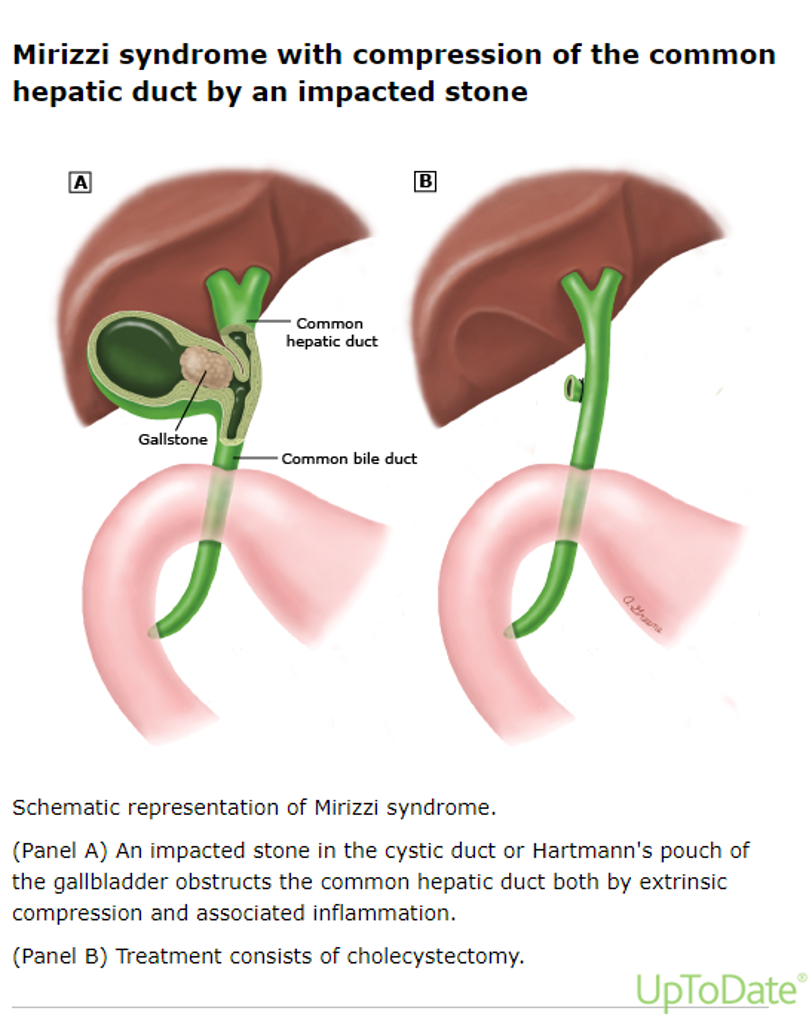
Case Presentation: A 62-year-old female presented with a two-week history of right upper quadrant abdominal pain radiating to the back. Her pain was described as sharp and intermittent and associated with subjective fever, nausea, vomiting, headache, and dizziness. On examination, the patient was hypertensive but afebrile. Abdominal tenderness was noted in the right upper quadrant with a positive Murphy’s sign. Lab studies were mostly unremarkable, with normal white blood cell count, bilirubin, and alkaline phosphate. An abdominal ultrasound was significant for a thickening of the gallbladder wall with associated pericholecystic fluid and a positive sonographic Murphy, cholelithiasis, and a fixed stone in the gallbladder neck. The patient was started on Piperacillin-Tazobactam for empiric coverage after blood cultures were drawn. General surgery and gastroenterology recommended performing magnetic resonance cholangiopancreatography (MRCP) to evaluate the biliary system. MRCP showed a large stone within the gallbladder neck measuring 1.8 x 1.4 cm, causing mild compression of the adjacent biliary duct and intra and extrahepatic biliary ductal prominence. Developing Mirizzi syndrome was suspected, and no choledocholithiasis was noted. Laparoscopic cholecystectomy was performed on day 4 of admission. Piperacillin-Tazobactam was continued for 24 hours postoperatively. The patient was discharged on postoperative day 2 without complications. The patient presented for surgical follow-up one week after discharge with no acute complaints, tolerating normal diet, and no signs of postoperative infection.
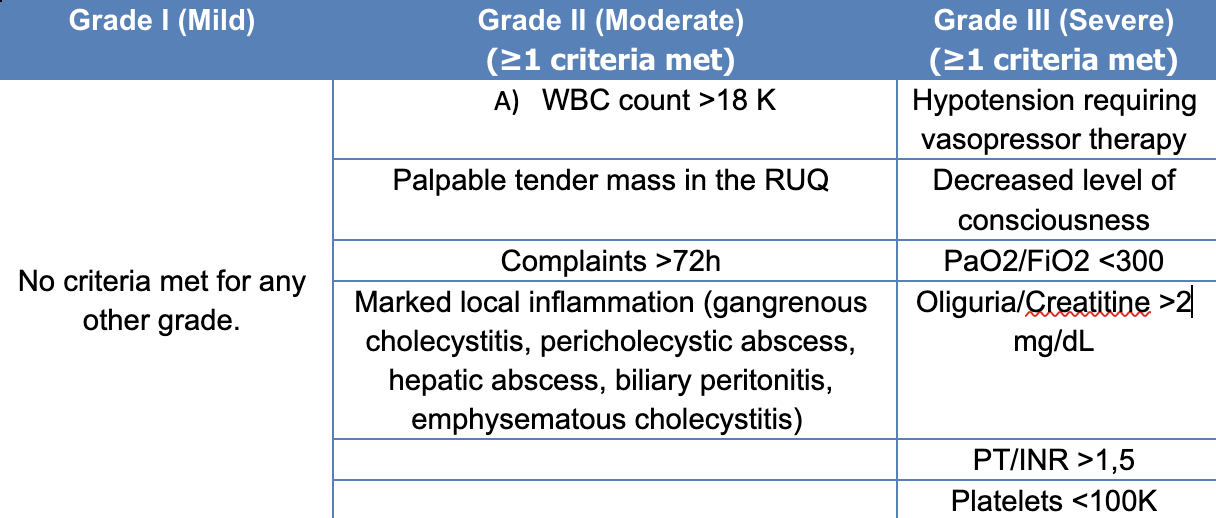
Discussion: Mirizzi syndrome is defined as a common hepatic duct obstruction caused by extrinsic compression from an impacted stone in the cystic duct or infundibulum of the gallbladder. (1) Although this is an infrequent finding, acute calculous cholecystitis is a frequent reason for admission. The 2018 Tokyo Guidelines provide diagnostic criteria and severity grading for the management of acute cholecystitis, and based on them, most cases are either mild or moderate. (2) (Table 1). Surgery remains the mainstay of treatment for acute calculous cholecystitis and Mirizzi syndrome. Antibiotic prophylaxis for surgical site infection has been shown to decrease complications, cost, and length of stay. (3) Further antibiotic administration should be guided by this classification of severity. Evidence supports similar outcomes for patients with Grade I or II calculous cholecystitis regardless of extended postoperative antibiotics. (4, 5) Unwarranted antibiotic use is known to promote multidrug-resistant bacteria, and this has been associated with increased adverse effects such as longer hospital stays, increased healthcare costs, and greater mortality. (6) This case met the criteria for grade II acute cholecystitis given the existing conditions of duration of complaints>72 hours and marked local inflammation. Since no evidence supported extending the duration of her antibiotic treatment, they were discontinued within 24h of surgery without adverse outcomes.
Conclusions: Antibiotic use in the postoperative period for acute calculous cholecystitis should be guided by its severity. Most cases are either mild or moderate, and evidence suggests no benefit from continuing antibiotics after surgical site infection prophylaxis is completed. Our case illustrates a successful application of the above recommendations in a patient with incipient Mirizzi syndrome.