Background: On March 7, New York was declared in “State of Emergency”; all Emergency Room and hospital facilities in NYC were overwhelmed by the rapid and high influx of patients with COVID-19 infection. At least 20% of patients with criteria for hospitalization received mechanical ventilation, and the Mortality reached 80% in a time when the only treatment option was oxygen support. South Bronx has a different population compared with other Boroughs in NYC. Disparities as income inequality, housing issue, and poor clinical care make this population unique to assess the clinical course and predictors of Mortality in mechanically ventilated patients (1,2). We aimed to evaluate baseline characteristics and clinical features as predictors for Mortality in mechanically ventilated patients due to severe COVID-19 infection.
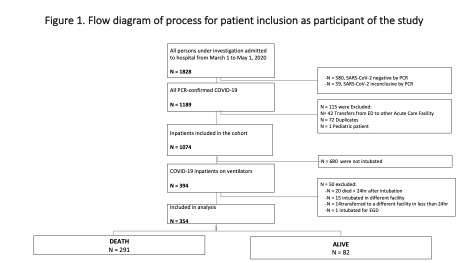
Methods: The retrospective cohort study included SARS-CoV2 positive patients by RT-PCR that underwent mechanical intubation during their hospital course between March-May 2020. Death in less than 24 hours after endotracheal intubation, patients intubated in the field, or transferred intubated from other facilities to our hospital were part of the exclusion criteria (figure 1). Simple logistic regression was performed to recognize variables for our model and Multiple logistic regression to identify covariates and cofounders for Mortality. A significant p-value was considered as <0.05. IBM SPSS v22 for Windows was used for analysis.
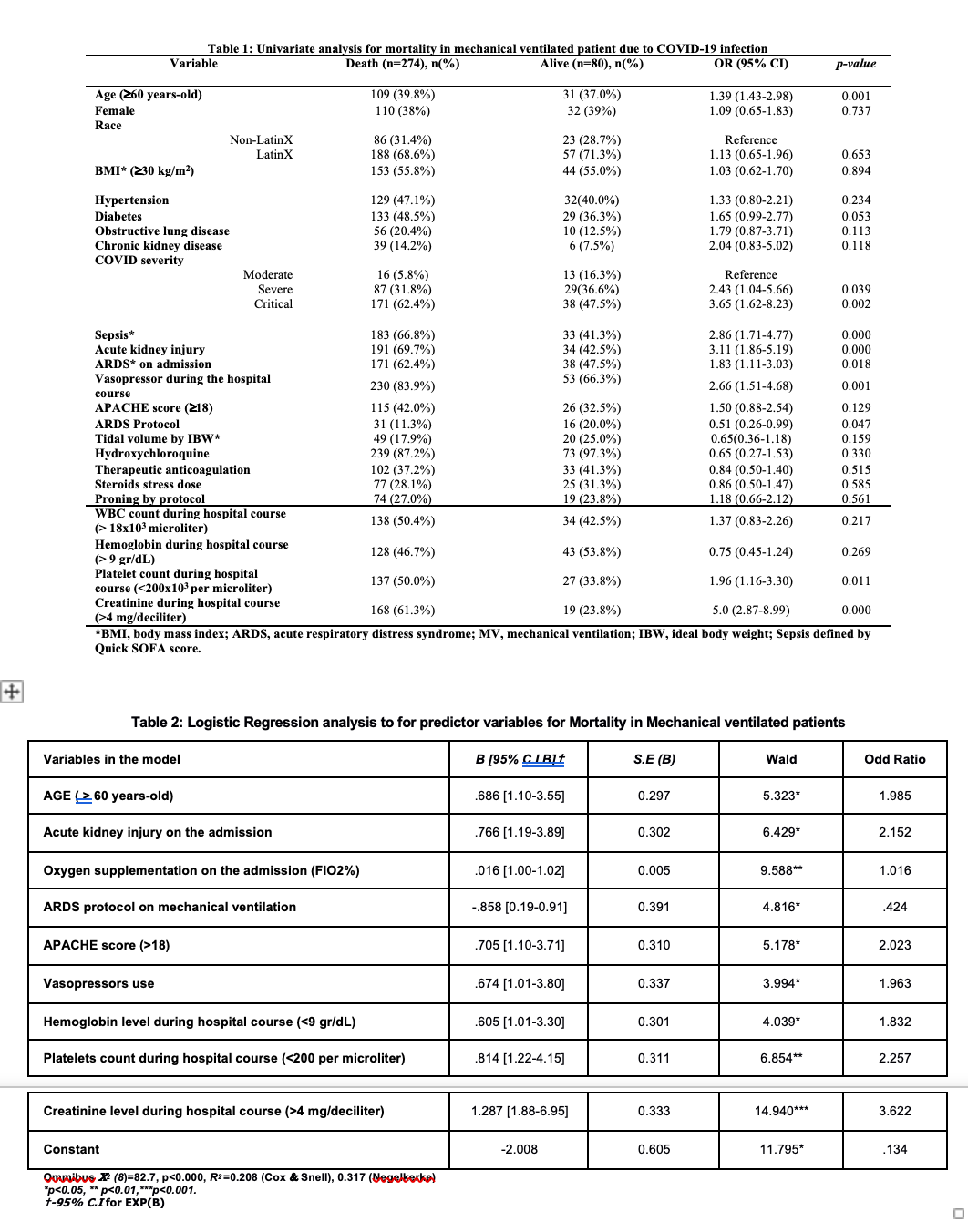
Results: Mortality in mechanically ventilated patients represents 82.2%. A list of clinically significant variables was evaluated in the Univariable Analysis (table 1) to determine our model’s set of variables among 354 subjects. A logistic regression analysis shows that there is a significant influence of age above 60, acute kidney injury on admission, level Oxygen Supplementation at the time of admission, use of vasopressors, APACHE score above 18; hemoglobin below 9 gr/dL, Platelets below 200, and creatinine level above 4 mg/dl during hospital course on Mortality of patient in mechanical ventilation (X2 (8)=82.7, p< 0.000). The model explained a 31.6% variance in Mortality in our sample (Negelkerke R2) and was able to identify 81.6% of cases accurately. The model's sensitivity was 38.8%, and the specificity of the model was 94.2 (table 2).
Conclusions: Mortality in mechanically ventilated patients in our cohort was high and did not differ from other studies in NYC (3). The WHO guidelines recommend mechanical ventilation support in COVID-19 infection for patients in ARDS or who need support for other dysfunctional organs. Older age, AKI, ARDS, and degree of oxygen support are independent predictors of mortality in critically ill patients with COVID-19 infection. SARS CoV-2 produces diffuse alveolar damage in the lungs that lead the patient toward ARDS. Therefore, ARDS protocol shows benefit in preventing Mortality among critically ill patients with COVID-19. This intervention assures enough oxygen levels in the lungs with poor compliance. It seems to be the only measure that improves Mortality among Mechanically Ventilated patients with COVID-19 infection (4-6).