Background:
Hospitals across the country struggle with improving patient experience and there is limited data on factors that drive positive or negative scores on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAPHS) survey. We sought to better understand which predictors may lead to a top box score.
Methods:
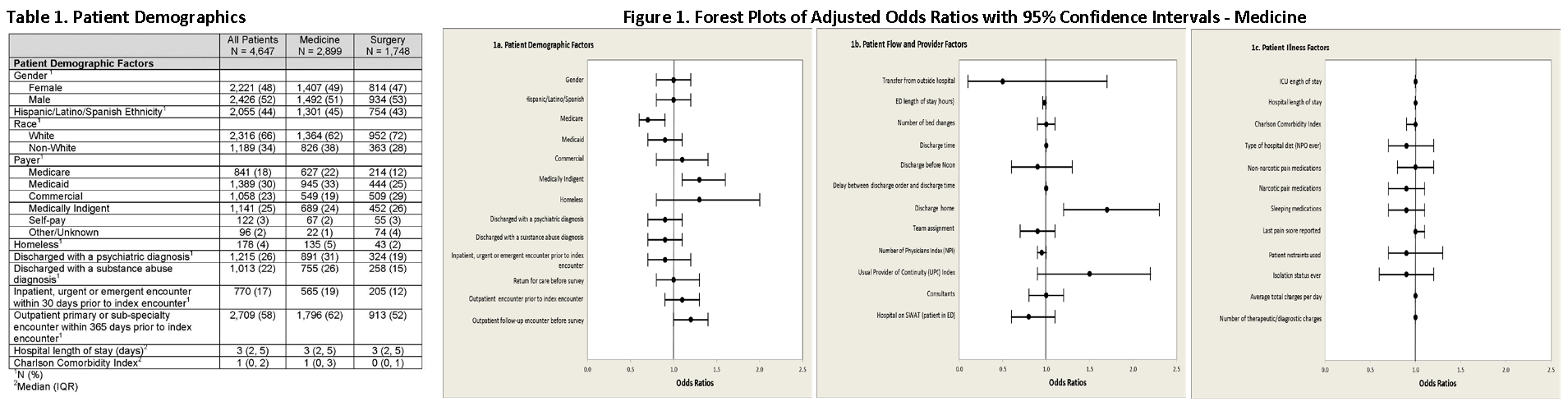
Administrative and clinical data were obtained for adult patients hospitalized at our institution, which is a public safety net teaching hospital with 525 beds, from August 2010 to May 2014, and had completed the HCAPHS survey. We studied patient demographic factors (i.e. gender, psychiatric illness), patient related flow factors (i.e. length of stay in emergency room, number of bed changes), and provider factors (i.e. continuity, teaching team). All predictors were selected a priori by consensus.
Unadjusted associations between selected variables and proportion top box (9 or 10) for the Overall Hospital Rating question were assessed using a Student’s t-test or a Wilcoxon Rank Sum test for continuous variables and a chi-square test for categorical variables. These covariates were then adjusted for the CAHPS Patient Mix Adjustment (PMA) factors (self-reported health status, education, non-English primary language, age, admitted through the ED, service line, and mean response percentile) using logistic regression. This study was approved by our Institutional Review Board.
Results:
Surveys from 4,647 patients were analyzed and demographics are shown in Table 1. After adjusting for the PMA factors, among medicine patients, the only variables associated with proportion top box for the overall hospital stay were insurance status (Medicare and medically indigent), and discharge disposition. Factors such as wait time, psychiatric diagnosis, substance abuse, lack of follow up appointments, number of bed changes, whether or not the patient received an opioid, etc. were not (Figure 1). For surgical patients, insurance status (commercial and medically indigent), psychiatric diagnoses, return for urgent, emergent, or inpatient care before survey, and number of bed changes were associated with proportion top box after adjustment (data not shown).
Conclusions:
The patient, provider, flow, and quality related metrics hypothesized to be associated with patient experience were not found to be related to a top box score for the majority of the variables studied. For the variables found to be significant, the majority are corrected for after applying the CAHPS PMA factors.