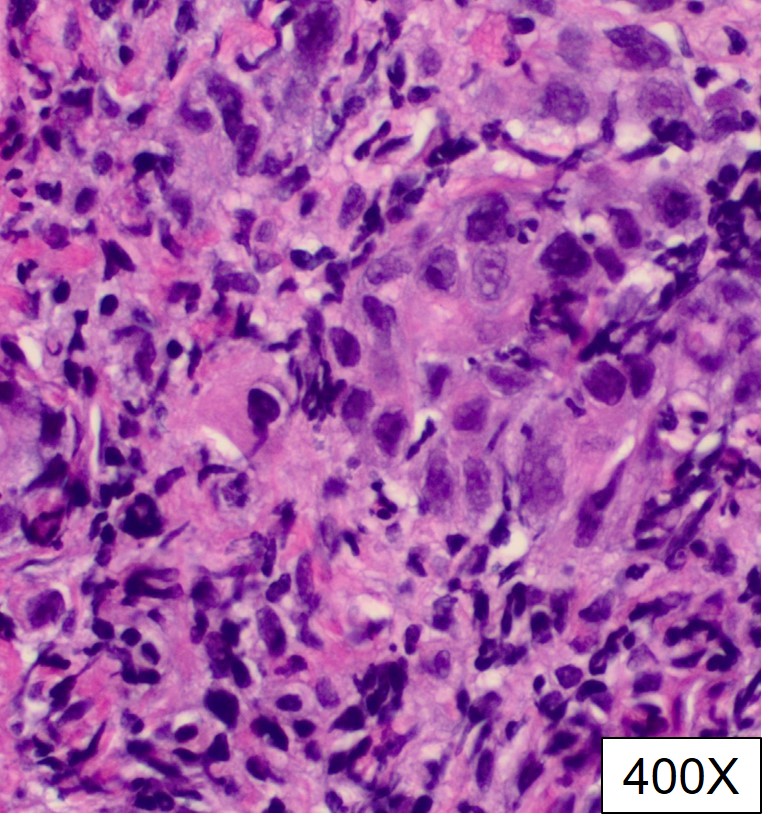
Case Presentation: A 34-year-old woman with history of celiac disease presented with diffuse abdominal pain for 3 days. She also experienced nausea and decrease appetite. There was nonspecific abdominal tenderness upon examination. Lab showed abnormal liver function test: alkaline phosphatase (561 U/L), GGT (632 U/L), ALT (149 U/L), AST (91 U/L), bilirubin (0.5 mg/dL). Abdominal ultrasound revealed dilated intra-hepatic and common bile duct 14mm with sludge but no gallstones, pericholecystic fluid or wall thickening. Magnetic resonance cholangiopancreatography (MRCP) found focal 18 mm lesion at the papilla of Vater with severe extrahepatic and moderate intrahepatic biliary dilatation. Biopsy and biliary sphincterotomy with stent placement were achieved with Endoscopic retrograde cholangiopancreatography (ERCP). Pathology study found invasive moderately differentiated adenocarcinoma. Immunohistochemistry (IC) stain was negative for MLH1, MSH2, MSH6, and PMS2. The patient underwent Whipple operation. Final staging was pT3bN1M0. Concurrent chemoradiotherapy with capecitabine was started. Subsequently the patient received adjuvant chemotherapy FOLFOX (Folinic acid (leucovorin), Fluorouracil (5-FU), Oxaliplatin (Eloxatin)) for 10 cycles. She had several repeat image studies every 3 to 6 months and no evidence of disease has been identified for 2 years after initial presentation.
Discussion: Primary ampullary tumor has low incidence of approximately four per million. It is thought to arise from adenoma, the benign precursor lesion, of the ampulla of Vater. Its pathohistology and biology behavior are similar to that of intestinal carcinomas rather than pancreaticobiliary cancers. The most common initial finding is obstructive jaundice. It can be difficult to distinguish primary ampullary tumor from the periampullary mass lesions with clinical manifestations and image studies. Sometimes the distinction between them can only be made until histopathologic study. It is crucial to have the optimal diagnosis and treatment approach because the favorable outcome of true ampullary cancer. ERCP is the most useful tool as it can identify the tumor, provide biopsy and decompressing stent placement. Ampullary cancer can be potentially recognized endoscopically. Whipple operation is the standard treatment for ampullary tumors. There is no well-established adjuvant therapy but some studies suggest adjuvant chemotherapy or chemoradiotherapy. Currently, there is no defined optimal surveillance. Most clinicians utilize CA19-9 or CEA and repeat CT scan every six months for the first five years.
Conclusions: It is important to identify primary ampullary cancer with ERCP and biopsy due to favorable prognosis. In addition to surgical resection, chemoradiotherapy or chemotherapy are widely accepted management. These patients should be followed with repeat tumor markers and image studies.