Background: Hospitalized patients are often cohorted on specific inpatient wards in an effort to improve outcomes and provider satisfaction. When hospitalist beds are fully occupied, patients may be admitted to off-service inpatient units. Dispersion to multiple units has the potential to affect multiple outcomes. Hospitalist groups may develop cohorting programs, either in the form of one team on one unit, or measures to reduce the total number of units visited by each hospitalist daily. The objectives of this study were to determine if a protocol to enhance hospitalist localization:1. Was effective at reducing dispersion. 2. Improved quality metrics.
Methods: This study was undertaken at an 711 bed academic medical center with 578 medical/surgical beds from June 2022 to July 2023. During this period, the hospitalist team had an average daily census of 255 patients. The hospital assigned beds to each non-critical care service across 21 units. Of those beds, hospital medicine had 152 assigned beds in 6 units, resulting in a gap of 103 medicine patient beds and perceived significant dispersion. An updated localization protocol was implemented in January 2023. Tactics included:1. Assessing bed capacity in each assigned medicine unit and average census on hospitalist teams. Home teams and primary units were reassigned to accommodate patient volumes.2. Location and census of overflow patients was determined based on #1. Home teams were assigned secondary units for overflow. Secondary units did not have assigned medicine beds, but had high medicine overflow census.The primary measured outcome was dispersion, defined as the number of different units in which hospitalists had patients. Secondary outcomes and balancing measures included length of stay index (LOS-I), mortality index, 72-hour readmissions, patient satisfaction scores, and care coordination rounds (CCR) attendance. Subjective provider input was also obtained via survey. A student’s t test was used for statistical analysis.
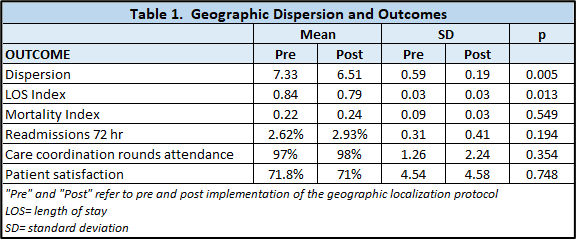
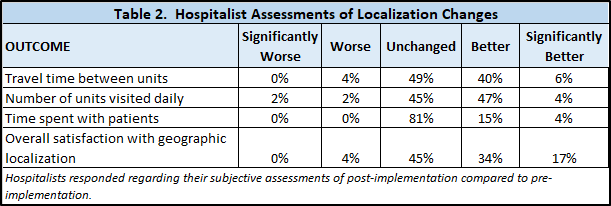
Results: Dispersion decreased after protocol implementation, with average dispersion pre-implementation of 7.33 units visited daily and post-implementation of 6.51 units, with a net difference of 0.82 (p< 0.005) (table1). LOS-I also decreased. There were no differences in mortality index, 72-hour readmissions, patient satisfaction, or CCR attendance (table 1). Thirty nine percent of hospitalists responded to a survey regarding the localization protocol, with the majority reported either improvements or no change in workflow and satisfaction (table 2).
Conclusions: This study demonstrated that a protocol to enhance hospitalist localization without adding newly assigned beds was effective at reducing dispersion. The overall impact was small, but statistically significant. This was additionally associated with a reduction in LOS-I, although causation cannot be directly known. Other metrics, including CCR attendance, mortality, readmissions, and patient satisfaction were not affected. Subjective assessment by hospitalist team members was either positive or neutral. It is possible that with larger reductions in dispersion, these measures may be more significantly impacted, so further interventions and study are required.