Case Presentation: A 28 year old woman with a history of metastatic adenocarcinoma and peritoneal carcinomatosis with partial bowel obstruction presented with 6 days of progressive nausea and vomiting. The patient also reported chest pain that was associated with retching and mild shortness of breath. She experienced change in vocal quality over the past few months noting that her voice was softer and higher pitched.Exam revealed BP 108/78, heart rate 140, respiratory rate 18, afebrile, and 98% oxygen saturation. It was significant for tachycardia without murmurs, clear lungs bilaterally, abdomen was mildly distended, tympanic with diffuse tenderness and hypoactive bowel sounds. Imaging was significant for extensive peritoneal and omental carcinomatosis without high grade obstruction and showed a normal esophagus. The patient was treated with antiemetics, IV fluids and soft diet.
On hospital day 2 the patient experienced worsening chest pain that was an aching pressure with progressive dyspnea that was prominent with conversation and her speech was hoarse and hypophonic. Oxygen saturation remained within normal limits and exam was unchanged.
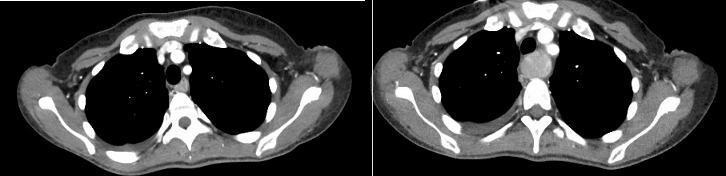
An EKG showed T wave inversions (not present on EKGs prior to this admission). A 2D echo revealed EF of 50%, normal RV and small LA from possible impingement due to an extra-cardiac mass. Repeat CT revealed a dilated esophagus that was impinging on the left atrium.
The patient underwent gastrointestinal decompression with NG tube for small bowel ileus with resolution of esophageal distension. The patient’s chest pain resolved immediately and the hoarseness and dyspnea resolved over the next 3 days.
Discussion: In a review of over 500 patients with recurrent laryngeal nerve paralysis, Yamada et al. found 3% of cases were caused by neoplasms, 30% by surgical intervention, 16% were idiopathic and 11% traumatic. Underlying cardiac disease is a small fraction of potential causes (4). We were able to only find 3 published case reports in which esophageal dilation led to vocal cord paralysis from recurrent laryngeal nerve palsy. One case was due to iatrogenic dilatation of an esophageal stricture (7). The second and third case were due to dilation of the cervical esophagus secondary to achalasia (6) and stricture (9). We were unable to find any cases related to peritoneal carcinomatosis causing ileus.
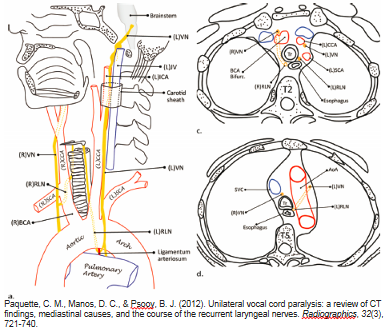
It was originally theorized by Ortner that an enlarged left atrium would compress the left recurrent laryngeal nerve against the aorta causing injury to the nerve. In our case, the injury to the recurrent laryngeal nerves most likely occurred in the tracheoesophageal groove. Our patient’s symptoms of dyspnea and hoarseness recovered in less than a week after gastrointestinal decompression. This is very similar to the previously mentioned achalasia and esophageal strictures cases of bilateral recurrent laryngeal nerve palsy secondary to esophageal distension. In both cases the vocal cords recovered due to quick intervention and decompression.
Conclusions: Our patient presented with dyspnea and dysphonia which are classic symptoms of recurrent layrngeal nerve palsy. Ortner’s syndrome is an uncommon cause of recurrent laryngeal nerve palsy and is associated with a dilated left atrium. Esophageal dilation remains an even rarer cause of recurrent laryngeal nerve palsy. This novel case of “Pseudo-Ortner Syndrome” further demonstrates the susceptibility of the laryngeal nerve to palsy secondary to mechanical impingement stemming from an unlikely distal non cardiac source.