Background: Geographic co-location, the practice of cohorting a panel of patients on the same hospital unit for a single provider or team, is increasingly popular, with 36.4% of adult hospitalist groups reporting unit-based assignments [1]. Benefits include increased hospitalist-patient interaction time, increased odds of multiple same-day patient visits, improved productivity, and greater interdisciplinary communication [2-4]. Associations with reduced mortality, length of stay, and costs were seen in bundled interventions [5,6]. Efficient throughput on Hospital Medicine (HM) teams is integral to facilitating timely access for inpatient care, especially when inpatient bed demand exceeds bed availability. However, the process of assigning patients to HM services in any open bed can generate an extensive footprint for hospitalists to cover, limiting time spent in direct patient care and communication with care team members (i.e., nurses, social workers). We sought to implement unit-level co-location of patients on HM general medicine teams to improve efficiency and throughput.
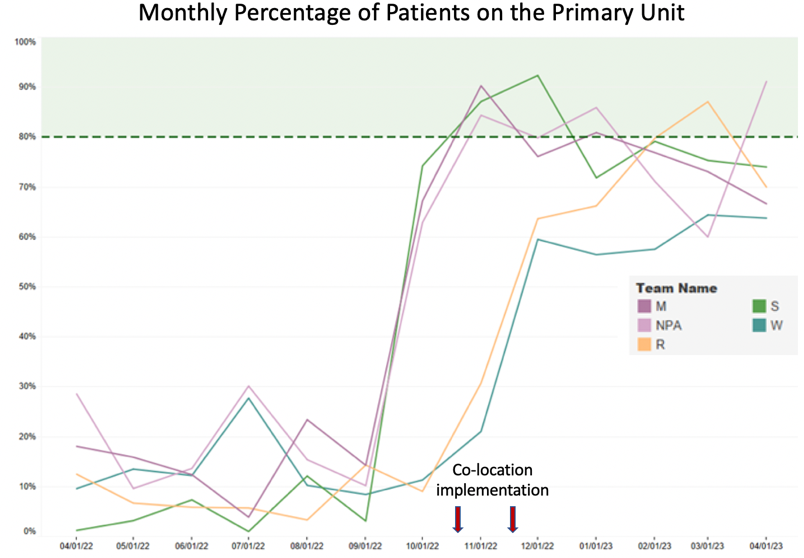
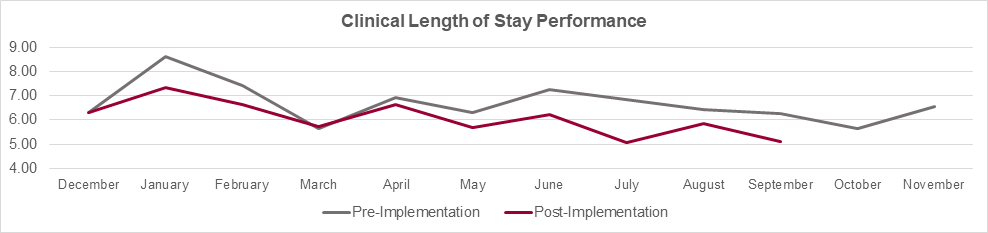
Methods: In this interdisciplinary quality improvement initiative, we implemented the co-location of hospitalist general medicine patients by teams, coupled with unit-based multi-disciplinary rounds (MDR). Other hospital initiatives including expansion of weekend procedures, restructuring of care coordination, and documentation improvement also occurred contemporaneously. Our interdisciplinary team included hospitalist physician leaders, nursing leaders, patient logistics director, and a project manager, with oversight from executive hospital leadership. An initial co-location proposal was drafted based on HM daily census, team capacities, beds per unit, and service structure. The HM teams were assigned to a primary unit, with an overflow plan to a secondary unit or pavilion. In the pilot phase, 3 teams were assigned to 2 adjacent units. In the expansion phase, 2 more teams were assigned to 2 additional units. A target of 80% of patients placed on the team’s primary unit was set as an indicator of effective co-location. Unit-based MDR was implemented once co-location reached a steady state near target. Additional tools were developed to maintain co-location efforts including daily huddles and secure messaging between HM Triage and Bed Access teams. Pre and post-comparison of clinical length of stay (LOS) and observed-to-expected LOS were conducted on patients discharged from the co-location units, December 2021 to September 2023. Balancing measures included case mix index (CMI) and readmissions.
Results: The average percent of patients on the primary unit for co-located HM teams improved from 11% to 74% (6 months pre/post-intervention, respectively). The monthly average over time is shown in Figure 1. The average monthly clinical LOS (Figure 2) and observed-to-expected LOS decreased by 10.3% and 22.2%, respectively. The monthly average case mix index was unchanged at 1.41 for the pre and post-intervention period. Readmission rates also remained stable.
Conclusions: Improvements in LOS suggest that creating closer proximity for HM teams to their patients can lead to greater efficiency in care delivery and improved throughput. However, other contemporaneous hospital interventions likely contributed to the substantial reduction in LOS. Additional efforts are ongoing in expanding co-localization and assessing clinicians and patient-centered metrics such as satisfaction scores and note completion time.