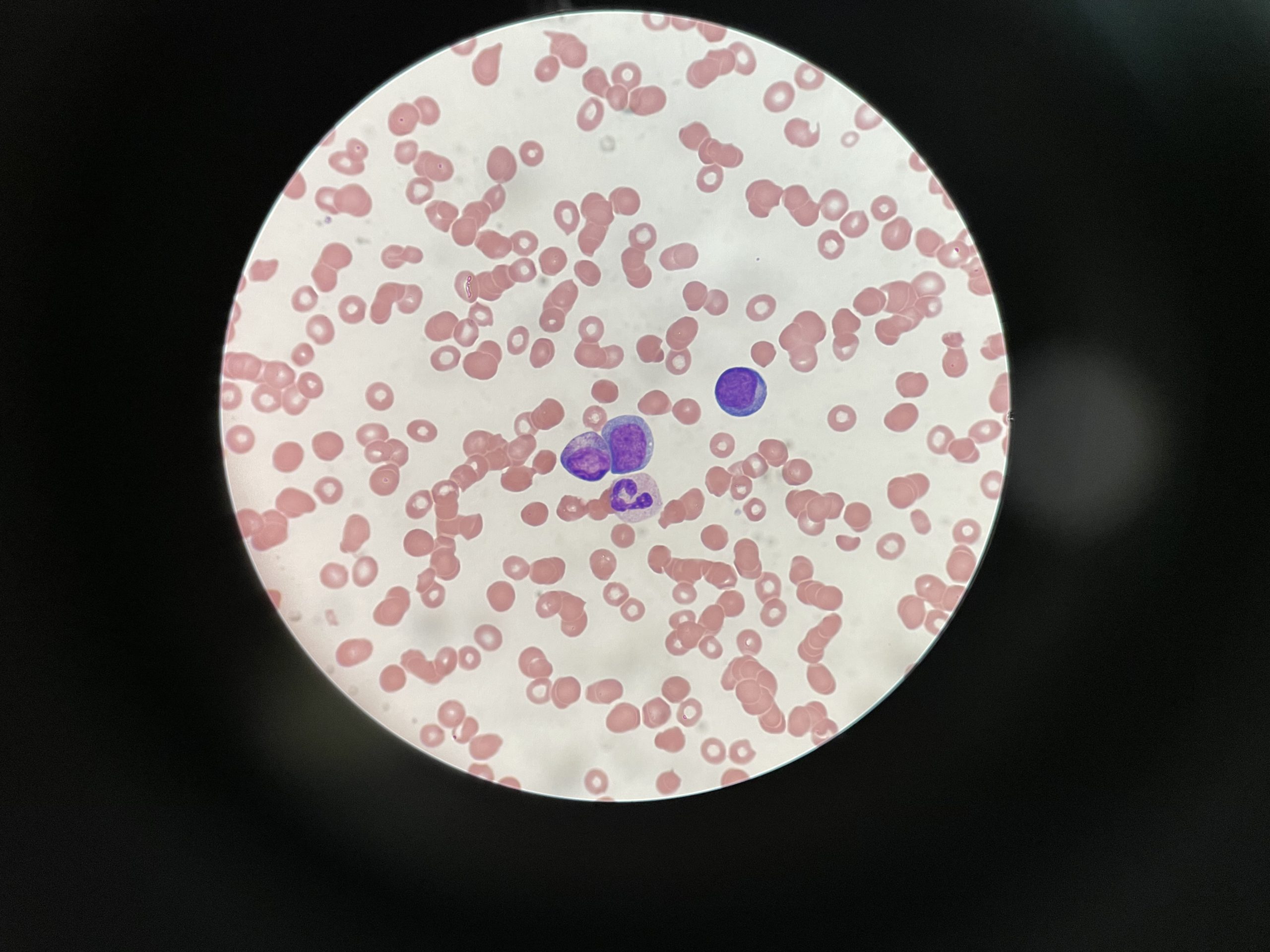
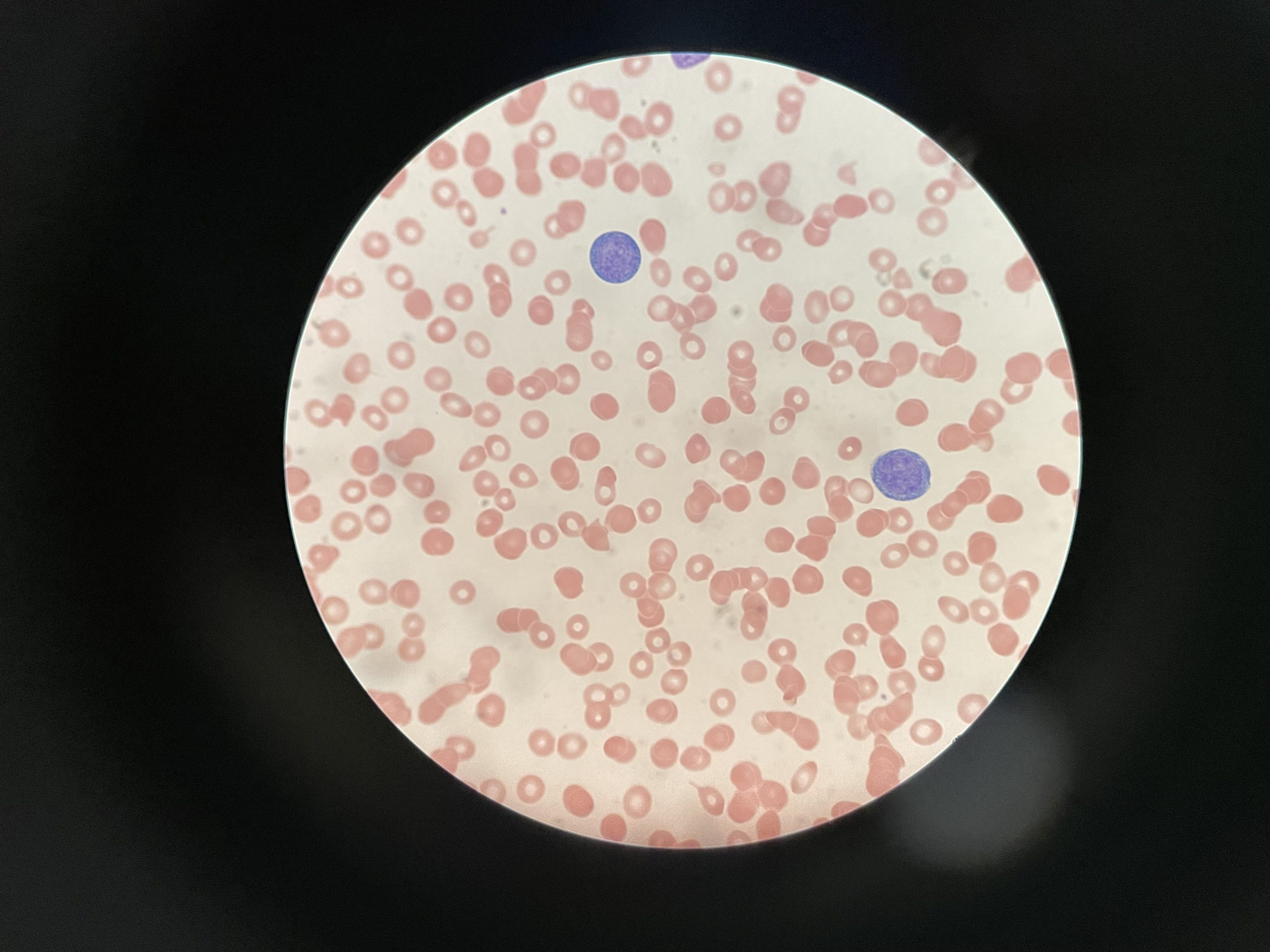
Case Presentation: We present the case of an 18-year-old female with no medical history presented to the emergency department with a two-day history of jaundice and dark-colored urine. She had no other typical symptoms of IM like sore throat, fever or flu-like symptoms. The only medication that she has been taking regularly is oral contraceptive pills (OCP). Physical exam was unremarkable except for bilateral conjunctival icterus and bilateral reactive axillary lymphadenopathy. Her laboratory workup was significant for the following: Aspartate aminotransferase (AST): 300 IU/LAlanine aminotransferase (ALT): 250 IU/LTotal bilirubin: 8 mg/dLDirect bilirubin: 3 mg/dLAlkaline phosphatase: 500 IU/LGamma-glutamyl transferase (GGT): 300 IU/LLactate Dehydrogenase (LDH): 500Haptoglobin: < 30 Differential diagnoses considered included OCP-induced cholestasis, biliary obstruction, hemolysis, and hepatitis. The hepatitis viral panel was negative, and abdominal ultrasound and magnetic resonance imaging ruled out biliary obstruction. Despite discontinuing OCP, liver enzyme and bilirubin levels continued to rise. Given elevated LDH and low haptoglobin levels, a direct Antiglobulin test was performed, confirming hemolytic anemia. A peripheral smear on admission showed RBC agglutination, dacrocytes and reactive lymphocytes. As part of the evaluation for hemolytic jaundice, the Epstein-Barr Virus (EBV) IgM antibody report was positive. Her symptoms and jaundice improved with supportive care, and she was discharged home with no need for any further treatment, hence was advised to resume the regular intake of OCP.
Discussion: EBV, a DNA virus primarily affecting the lymphoreticular system, commonly infects adolescents and young adults. IM is characterized by lymphocytosis, with a predominance of CD8+ cytotoxic T cells. Some IM complications arise from EBV-induced production of antibodies targeting red blood cells, white blood cells, and platelets. Hemolytic anemia, often associated with anti-I cold agglutinins, is usually IgM-mediated. Elevated aminotransferases are a common finding, usually self-limiting, but a cholestatic jaundice pattern is rare. Significant cholestasis and jaundice are rare complications with an incidence of less than 5%. In a literature review (2005) , there were only 24 cases of cholestatic hepatitis [1]. IM should be considered in the differential diagnosis, particularly in young adults, when encountering mixed direct and indirect bilirubinemia pattern [2]. While heterophile antibody titers may be negative initially and persistently in approximately 10% of cases, EBV viral capsid antigen IgG and IgM antibody testing should also be performed [3]. EBV-related complications can range from mild hepatitis to more severe conditions like fulminant liver failure [4], necessitating close follow-up, although most cases resolve with symptomatic management.
Conclusions: We report the case of IM with a rare complication of indirect and direct hyperbilirubinemia. EBV-related jaundice is a rare complication of IM. It is essential to consider IM in patients presenting with jaundice, especially in young adults without typical IM symptoms. IM-related cholestasis jaundice should be managed with supportive care and must be monitored closely due to reported fulminant liver failure consequences . Future research should focus on identifying risk factors and effective treatments for EBV-related jaundice.