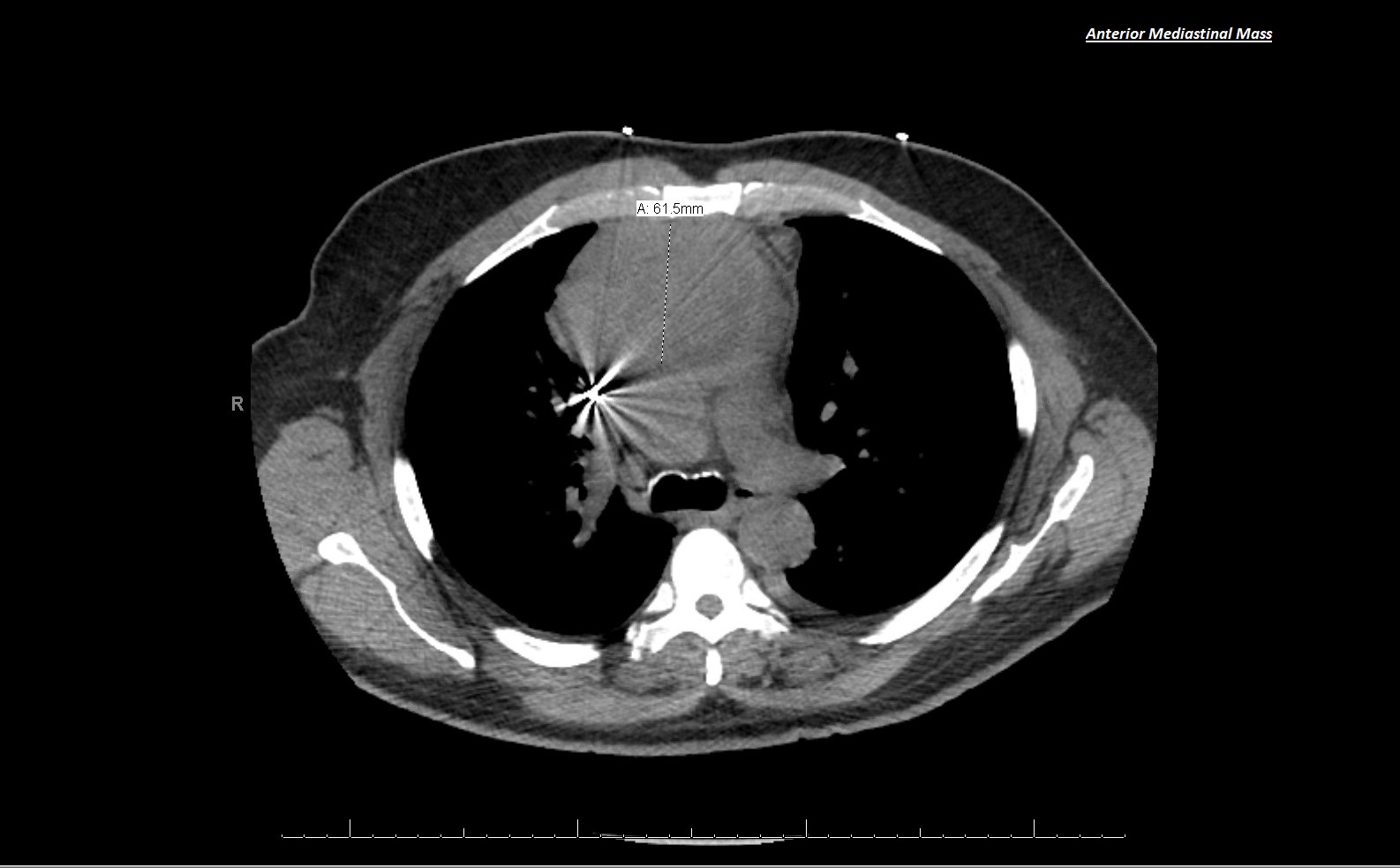
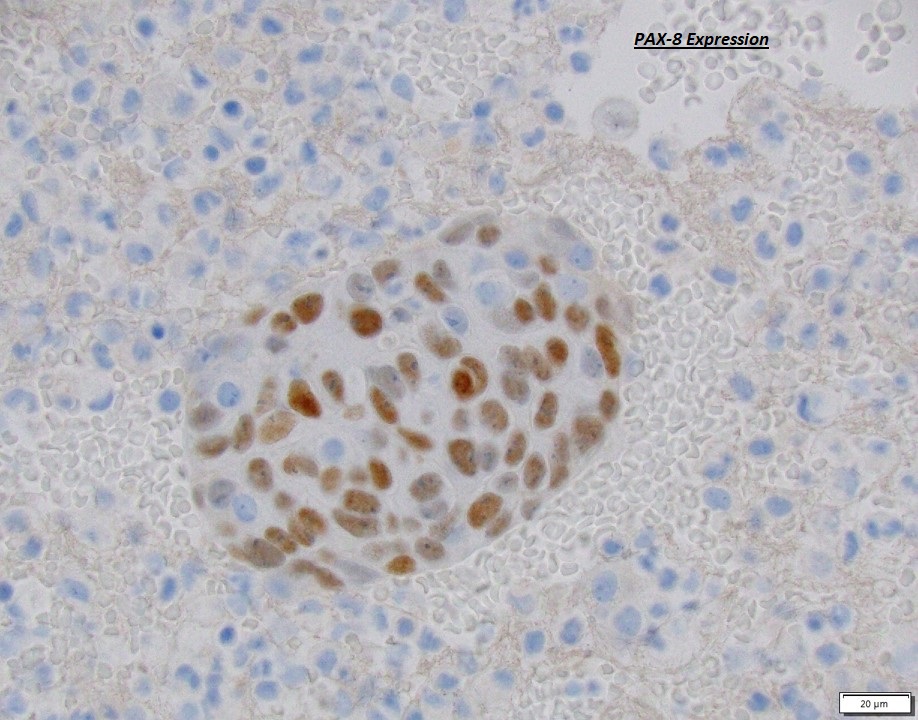
Case Presentation: Our patient is 56-year-old gentlemen with a history of non-ischemic cardiomyopathy related to prior alcohol use, hypertension and atrial fibrillation who presented to the emergency department complaining of shortness of breath, pleuritic chest pain and subjective feeling of fever and chills of 3 days’ duration. He was found to be hypotensive (86/60 mmHg) and tachycardic (120 bpm) but otherwise afebrile with normal pulse-oximetry on room air. Distant heart sounds and jugular venous distention were appreciated on physical examination. Chest X-ray showed cardiomegaly however his labs and electrocardiogram were largely unchanged from previous studies. Given the significant concern for cardiac tamponade, bedside transthoracic echocardiography was obtained which demonstrated a large pericardial effusion with signs of tamponade for which he underwent emergent pericardiocentesis with subsequent removal of 600ml of serosanguinous fluid. After hemodynamic stabilization, he underwent computed tomography of the chest which revealed an anterior mediastinal mass measuring 6.2 X 10.2 X 6.5 cm with scattered calcifications and extensive mediastinal and epicardial lymphadenopathy. Cytologic evaluation of the effusion revealed poorly differentiated Squamous Carcinoma of Thymic origin (non-keratinizing squamous-cell carcinoma) which was later corroborated by surgical biopsy. Despite aggressive chemoradiotherapy, the patient passed away approximately a year after diagnosis.
Discussion: Acute cardiac tamponade is a life threatening medical emergency that requires prompt identification and treatment in the form of pericardiocentesis. Most cases are idiopathic and are attributed to viral infection, however, a thorough evaluation is important as 25% of pericardial effusions are associated with malignancy (1), with breast and lung cancer being most common, followed by lymphoma and leukemia. Although tumors of the thymus are rare in adults, representing only 1% of all malignancies – they are the most common cause of an anterior mediastinal mass (2). Thymic carcinomas being the rarest subset of thymic tumors, mostly present as dull aching chest pain, cough, hoarseness, phrenic nerve palsy or Superior vena cava syndrome (3). Pericardial effusion causing cardiac tamponade is a very rare presentation of thymic carcinoma. Scarce data is available regarding the epidemiology and risk factors related to thymic cancers, but previous studies suggested an association with chest radiation and Epstein-Barr virus (EBV) infection (4). Prognosis in advanced forms of thymic cancer is poor with a 5-year survival of 40% despite appropraite surgical and medical interventions(4).
Conclusions: We present a case of rare thymic cancer manifesting as an acute cardiac tamponade with hemodynamic compromise in a previously asymptomatic patient. Prompt identification of signs and symptoms of cardiac tamponade is extremely important to decrease immediate mortality. Although the diagnosis of tamponade is clinical, bedside echocardiography is a rapid and reliable means to diagnose effusion and tamponade. Further evaluation of pericardial fluid including cytology and imaging is important as 1/4th of the cases can be associated with malignancy.