Background: Physician turnover is associated with poor morale and low job satisfaction. Turnover is costly to hospital systems and provider groups given decline in productivity, need for expensive alternative staffing, and increased recruitment efforts. Physician groups with high turnover and low job satisfaction lack the ability to gain traction on quality improvement work reflected in low levels of physician engagement. While national trends regarding physician administrative full time equivalents (FTE) are known, the optimal number for a group is unknown. Appropriately staffed physician administrators contribute to hospital group health without excessive administrative cost.
Purpose: This project aimed to describe one center’s experience with hospitalist team stabilization and upfront associated physician administrative FTE investment evaluating the effect on system cost savings and physician job satisfaction.
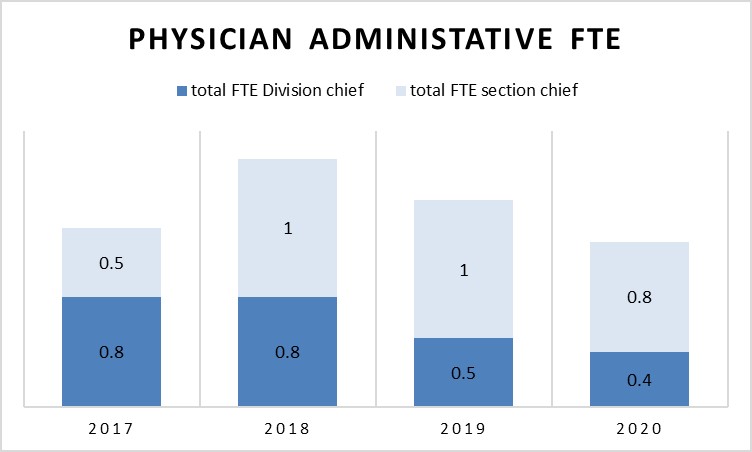
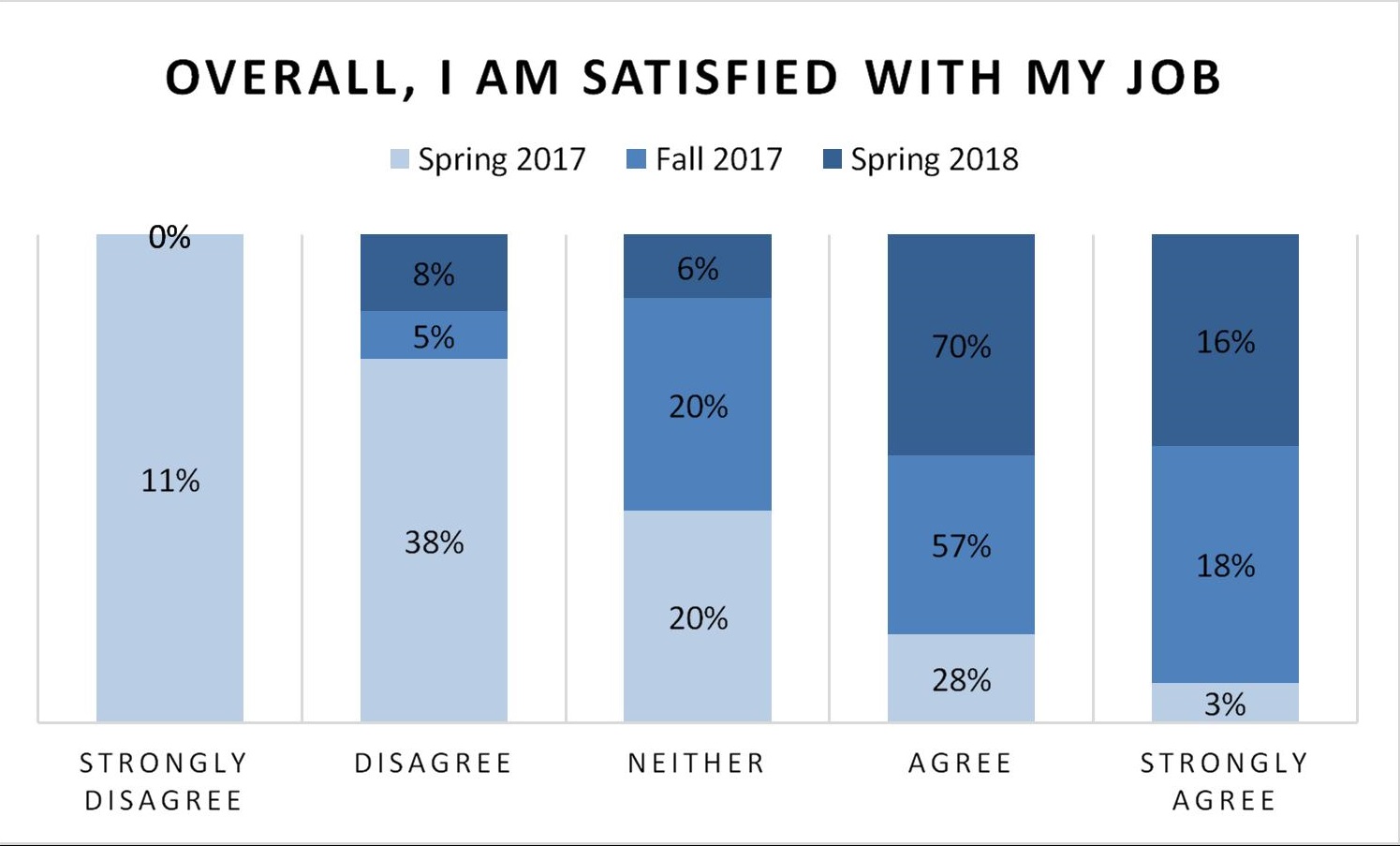
Description: In 2017, a 100-member hospitalist group had a turnover rate of 18%.Low levels of job satisfaction were noted with 31% of providers agreeing or strongly agreeing to the survey statement “overall I am satisfied with my job”. 49%t of providers disagreed or strongly disagreed to the same. Locum physicians were employed to cover staffing deficiencies of 9.5 FTE.To address these issues, physician administrative FTE was expanded from 1.3 FTE between 3 administrators to 1.8 between 5 administrators in late 2017 (Figure 1). This allowed for increased administrator led work including time for frequent direct physician leader to physician meetings, rapid attention to developing issues, increased recruitment efforts, wellness initiatives, quality project development, billing education, and co-management agreements.With upfront physician administrative FTE investment and subsequent interventions, locum staffing was eliminated. Overall job satisfaction increased from 31% in the spring of 2017 to 86% in the spring of 2018. Job dissatisfaction decreased from 49% to 8% (Figure 2). Hospitalist career advancement opportunities increased during period of stabilization as well as engagement defined as hospitalist lead initiatives and quality work. System length of stay (LOS) decreased by an estimated 0.5 days during this time. No additional operational support was provided during this time to account for changes noted. Hospitalist turnover has decreased to 3% by 2019, 40% below national average. Cost savings include the elimination of Locum physicians (~ $3 million/year), decrease in LOS (> $60 million/year), as well as recruitment and onboarding savings ($100K/physician), results of quality improvement work (> $2million/year).Physician administrative FTE has subsequently been decreased to lower than initial level after group stabilization by late 2019 (Figure 1).
Conclusions: High turnover and low job satisfaction are fundamental barriers to improvement of hospitalist group performance. Efforts made possible by short term physician administrative FTE investment resulted in improved job satisfaction and engagement, decreased turnover, elimination of locum use, and increased career advancement opportunities. Significant cost savings for small upfront hospitalist physician administrative FTE investment can be achieved. Most substantial cost savings resulted from elimination of locum staff and benefits of lower turnover and improved performance. Appropriate administrative FTE is important to the health of a hospitalist division, especially during periods of growth.