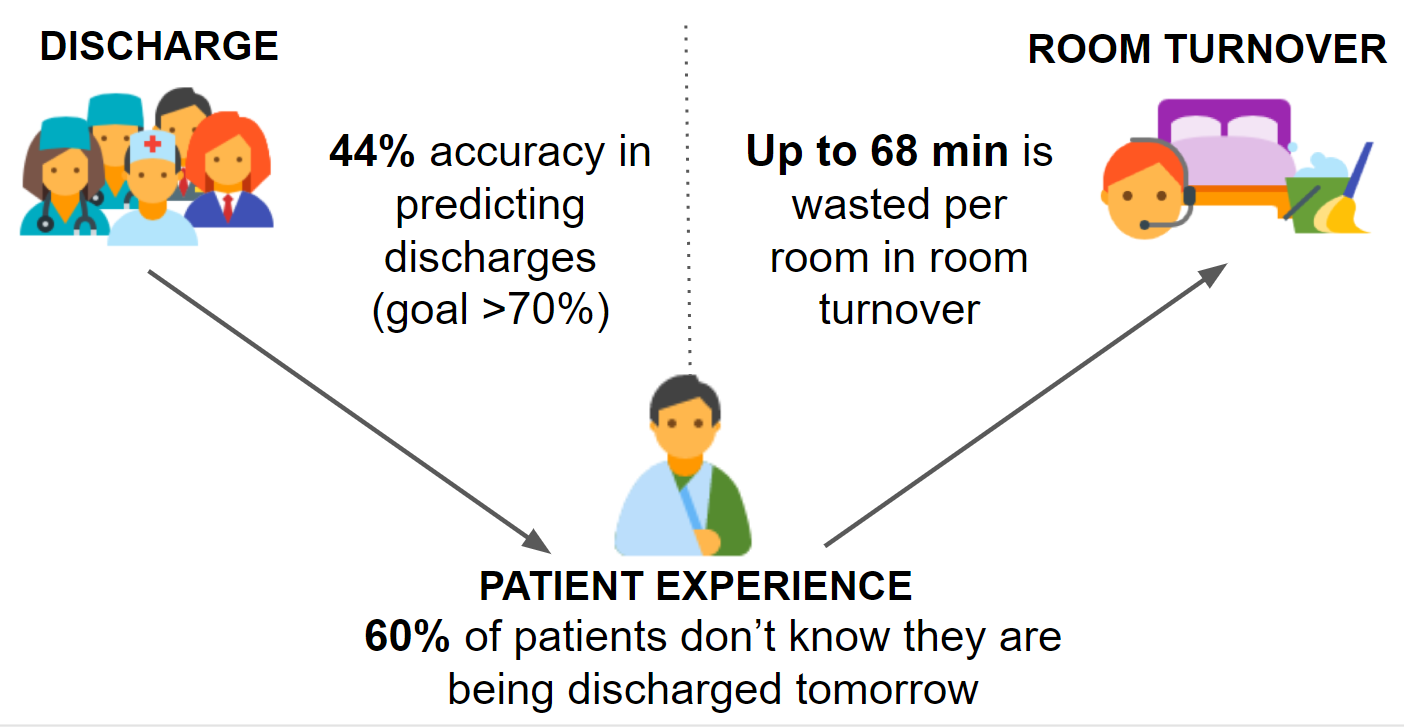
Background: As a group of medical students in a five-week leadership program, we were charged with making a medicine inpatient unit at an urban quaternary care academic medical center the best unit in the hospital. Research shows that the hospital spends an estimated $2721 for every inpatient day (Kaiser, AHA Annual Survey, 2015). Longer lengths of stay and emergency department times are associated with increased patient mortality and reduced hospital reimbursement (Hall et al., NCHS data brief, 2013). In order to reduce patient’s length of stay and wait time, we focused on the barriers and inefficiencies to discharge and room turnover. We interviewed ten unit staff and thirteen patients and timed ten discharges and room turnovers. We found that providers are 44% accurate at predicting next-day discharges, 60% of identified patients do not know they are being discharged the next day, and it can take up to 68 minutes before the hospital is informed that the discharged patient left the unit.
Purpose: This study aims to improve the accuracy of discharge predictions, reduce discharge delays related to patient preparedness, and reduce room turnover time. This will improve hospital flow thereby reducing wait times and lengths of stay.
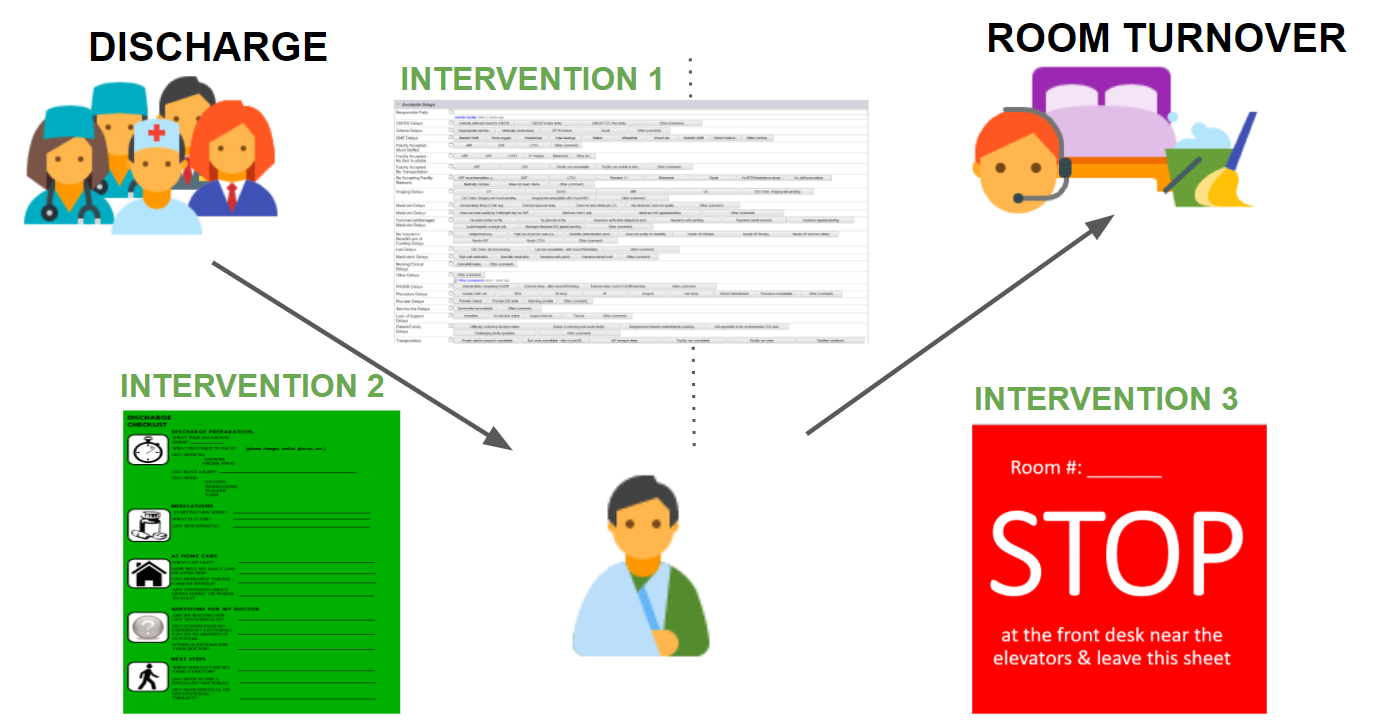
Description: We implemented a Discharge Delay tracker, a patient-centered Discharge Checklist given to next-day discharges, and a form that discharging patients leave at the front desk indicating they left the unit. Discharge delays were tracked (n=15) and events in the room turnover process were timed before (n=9) and after our interventions (n=10). This study had three main findings: 1) 27% of discharge delays are due to changes in patient’s medical status, 2) utilizing a patient-centered Discharge Checklist can reduce delayed discharges by 24%, and 3) eliminating communication requirements among unit staff can lead to a 16% average reduction in room turnover time.
Conclusions: Based on these findings, this study concludes that there is significant, reducible waste in the discharge and room turnover processes. Some approaches to reduce this waste include 1) tracking avoidable discharge delays to identify trends and improve prediction accuracy, 2) giving patients a Discharge Checklist to make them more aware, satisfied, and prepared for discharge, and 3) addressing communication inefficiencies to reduce room turnover time. These interventions can be implemented at other institutions and should be continuously reevaluated and improved.