Background: COPD exacerbations are among the leading causes of hospital readmissions. According to the COPD Foundation, in 2013, 22% patients admitted for COPD exacerbation required readmission within 30 days of discharge. This represents a significant burden in terms of morbidity for these patients and increased cost to the healthcare system. The COPD readmission rate during January to March 2016 at our institution was 15.2%. Our aim was to develop and test an intervention to decrease readmission rates for patients admitted for COPD exacerbation by 5% during the same months the following year.
Methods: Using the Define/Measure/Analyze/Improve/Control (DMAIC) model for quality improvement, input was obtained from identified stakeholders including physicians, nurses, social workers, and respiratory therapists (RT). The main factors that were identified in these discussions were lack of patient education and gaps in post-hospitalization follow-up. We implemented the following interventions: (a) Evaluation by an RT within 24 hours of admission with COPD teaching (tobacco cessation, nebulizer use/cleaning, home oxygen use, medications and recognition of symptom worsening) (b) Follow-up on day of discharge using the “teach-back” method to ensure patient understanding; (c) At least one follow-up phone call after discharge. The sources utilized were readmission data collected and reported by the Centers for Medicare and Medicaid, our institution’s electronic medical record, and RT logs.
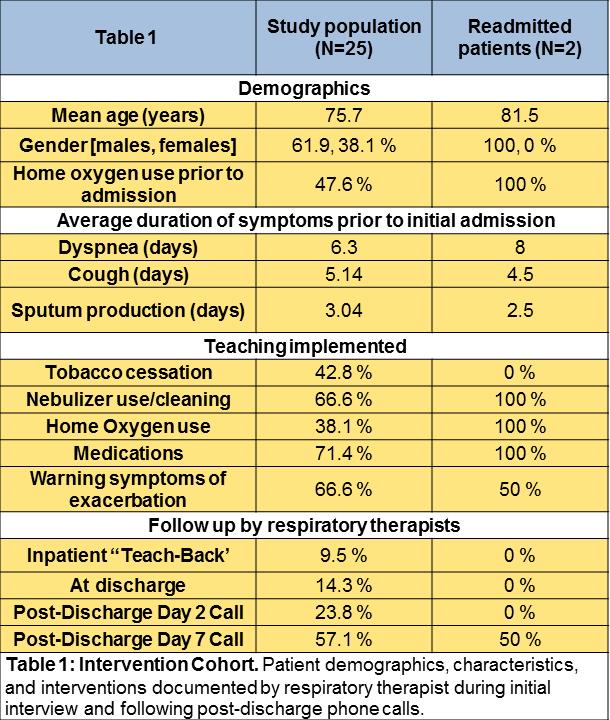
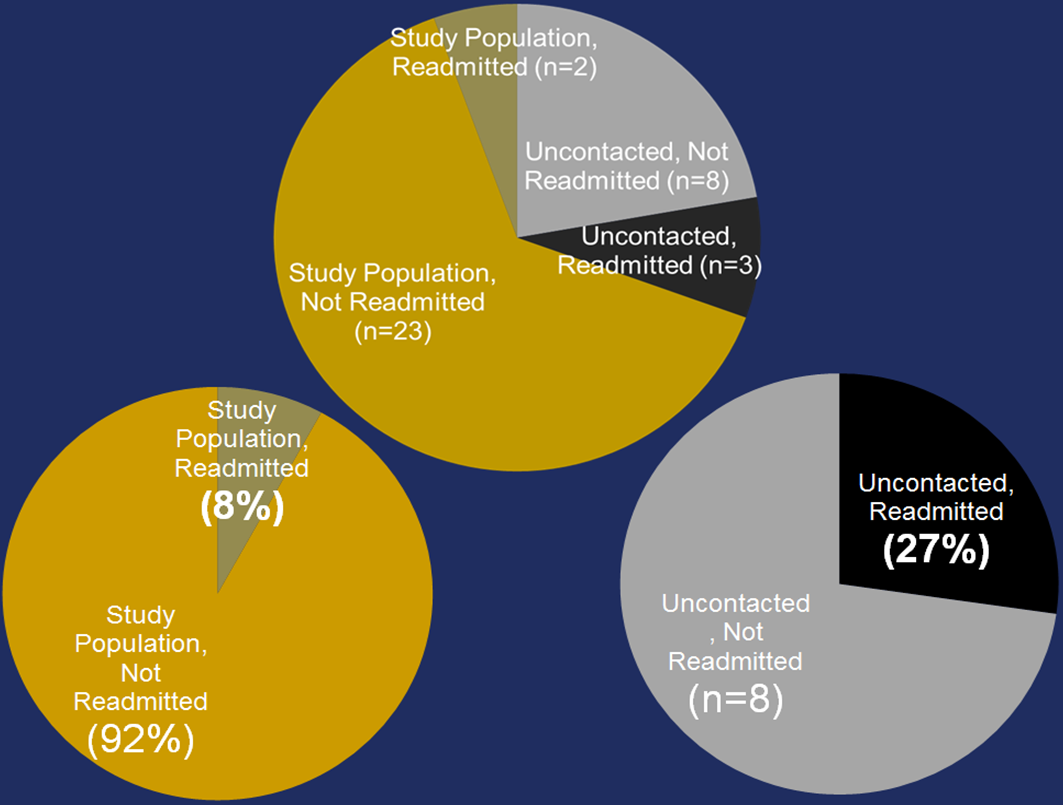
Results: We identified 36 patients admitted for COPD exacerbations over a 90 day period in the winter of 2017. Of these patients, 25 (69%) were approached for the initial interview. 2 (8%) of the 25 were readmitted within 30 days. Of the 11 patients who were unable to be reached, 3 (27%) were readmitted within 30 days. Readmission risk factors identified were age, male gender, home oxygen use, and duration of dyspnea before presentation [Table 1]. While overall readmission rates showed no remarkable changes (14.3% vs 15.2%), rates among patients who received the intervention was significantly lower than the control cohort (8% vs 27%),. Notably, 5 patients in the intervention cohort were COPD readmissions from previous hospitalizations within 30 days, and none were readmitted after the intervention.
Conclusions: We found that COPD readmissions were reduced by improving the quality of patient education provided during their hospitalization and by instituting systematic post-hospitalization follow-up calls. Wider implementation of this intervention, if applied to a greater number of patients, could be effective in reducing overall COPD readmission rates.