Background: Telemetry utilization for a long time has been dependent on individual physician experiences, preference as there were no good randomized controlled trails or guidelines from any scientific organization. American Heart Association has released the guidelines for appropriate use of telemetry in Oct 2004. Even more than a decade of these guidelines been available there has been significant overutilization of telemetry in various facilities. Research showed that when a patient is on telemetry Hospitalist only know 48% of the times, Interns 12%, Residents 18% and Teaching attending 9% of the times . This lead to keeping patients longer than intended and will lead to working up artifacts. Even though patients are not charged separately for Telemetry it costs about $ 53 per patient day.
Purpose: We at JMH faced challenges with lack of telemetry monitors at times and needed to borrow from our peripheral facilities which was a hassle. Also we had to invest additional resources in monitoring numerous telemetry screens and nursing on bed side with trying to fix the detached telemetry leads, assisting patients get up from bed, reviewing telemetry strips daily on all these patients. Patient experience was also hampered with these attached to their chest and restricting their mobility and disturbing their sleep. Telemetry was one of the frequent reasons for patient’s discontent.
Description: Design of project: 1) Education: We have conducted education sessions for residents. Hospitalists, ED and nursing.
Class I: at risk of an immediate, life-threatening arrhythmia—typically ICU appropriate patients (i.e. patients in the first 48 hours of ACS or with high grade lesions awaiting intervention, acute heart failure, 2nd and 3rd degree AV block, temporary pacing, long QT syndrome, WPW with rapid anterograde conduction, IABP, post cardiac arrest, post cardiac surgery, post-PCI or ablation with complication, post pacemaker placement.
•Class II: individuals presenting with chest pain syndromes, syncope, known arrhythmia with active arrhythmia medication titration, heart failure, and post-PCI, post-ablation or post-pacemaker placement without complications.
•Class III: includes rate-controlled atrial fibrillation, chronic PVCs, ESRD on HD and low risk post-surgical patients
2) Clinical Decision support/ alerts on Electronic Medical Records: based on ACC guidelines.
3) Modified non-evidence based telemetry orders: .
4) Posters:
5) Monthly review of data and provide the educational resources.
6) Telemetry techs to remind Physicians: One of the challenges that we were initially facing was forgetting to discontinue telemetry once started and so we have developed a standard of work for the telemetry technicians who would call at 2pm to all the hospitalists and residents reminding of patients on telemetry. Hospitalists, residents would in turn discontinue the telem
RESULTS ;
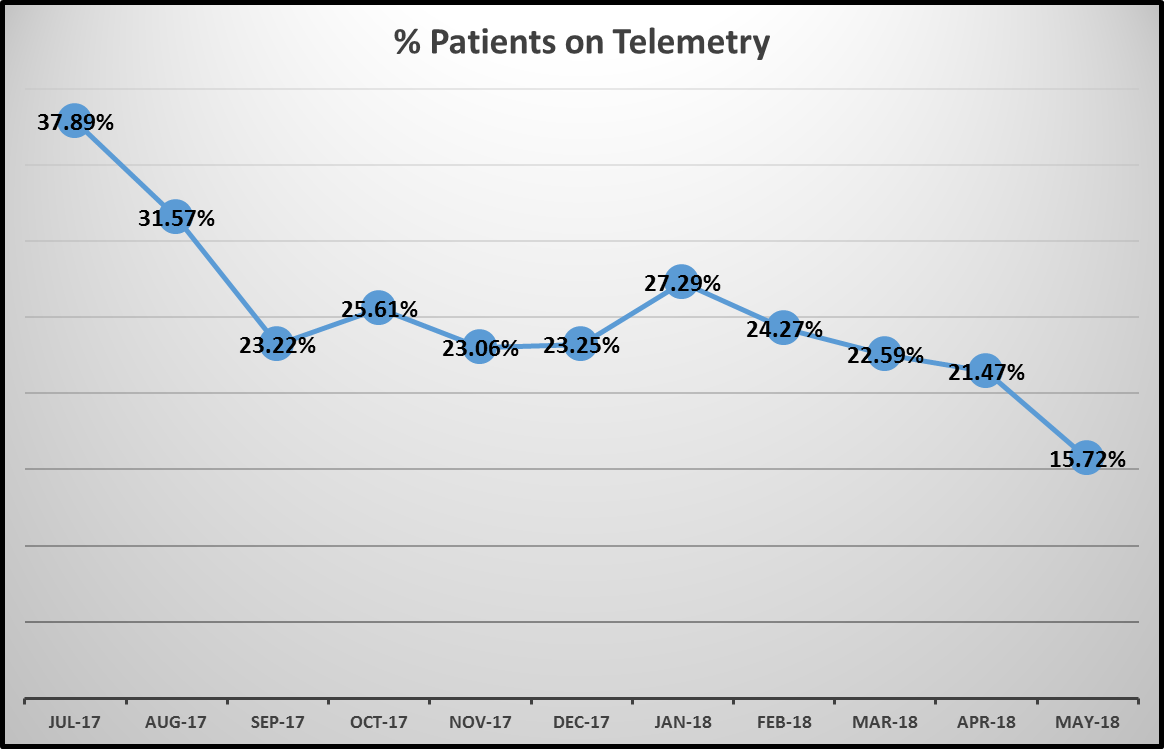
1) Reduction in telemetry utilization of 59% (38% utilization to 15.7% utilization from July 2017 to May 2018.
2) Reduction in cumulative length of time patients were on telemetry reduced by 58%.
3) Number of Code Blues – 34 in FY 2017 and 31 in FY 2018 indicating no compromise in care
Conclusions: Telemetry has been universally over utilized inappropriately and has resulted in increased cost of care, excessive use of resources, inconvenience to patients and offering no additional advantage. Practicing evidence based telemetry utilization, reduced 59% utilization and no harm to the patients.