Background: Inappropriate diagnosis of urinary tract infections (UTI) contributes to antibiotic overuse. We previously validated and refined a patient safety measure that defines inappropriate diagnosis of UTI (i.e., treatment of asymptomatic bacteriuria [ASB]) and was endorsed by the National Quality Forum. Use of this measure as a pay-for-performance metric in the Michigan Hospital Medicine Safety consortium, a group of 69 Michigan hospitals of which >75% have >100 beds), resulted in significantly reduced ASB treatment. Because little is known about the impact of diagnostic error in critical access hospitals (< 25 beds), settings that usually have fewer resources for stewardship, we aimed to determine if the measure could be implemented to reduce ASB treatment in this group.
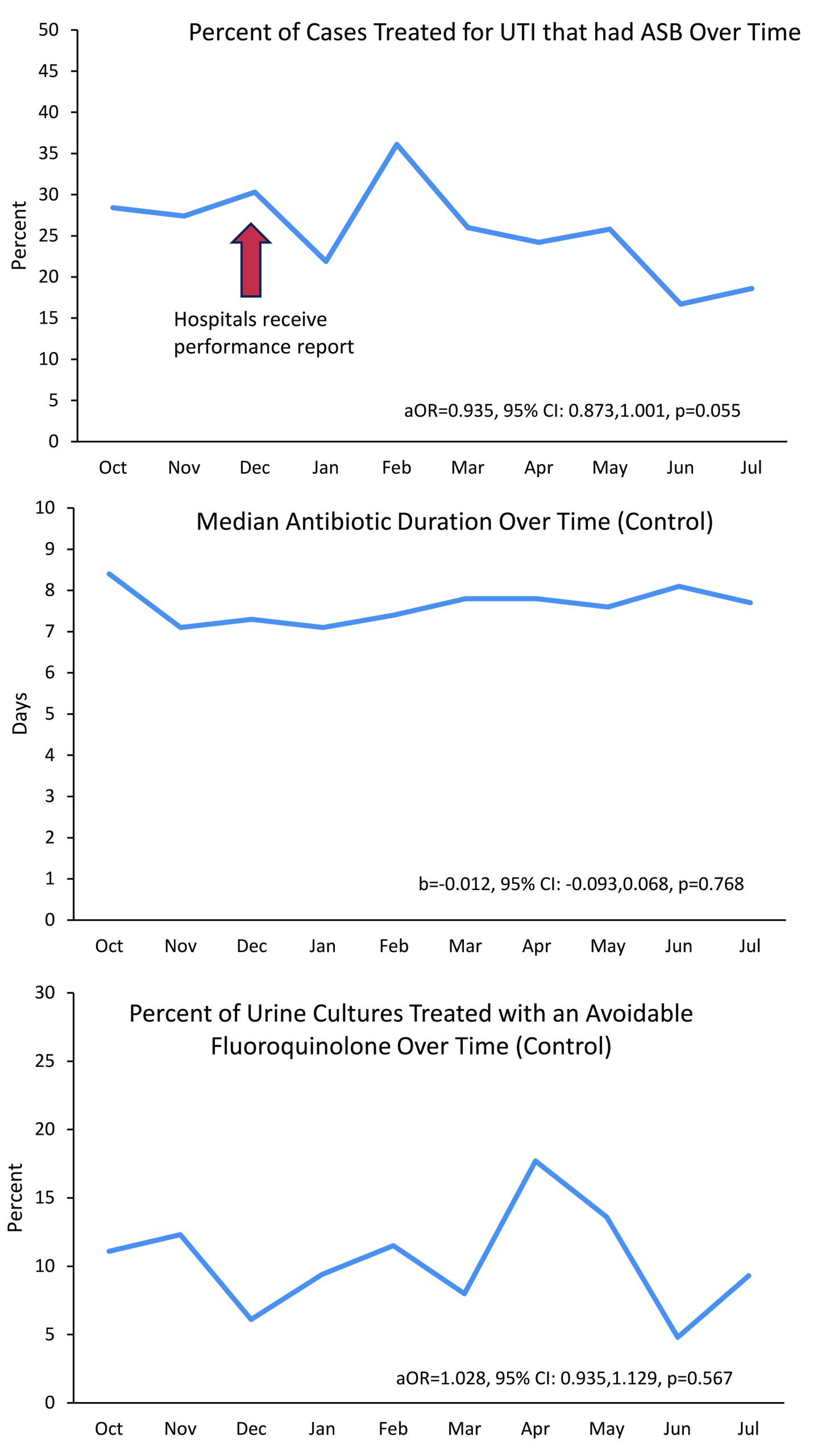
Methods: From October 2022 to July 2023, ten critical access hospitals from the mountain west participated in an Intensive Quality Improvement Cohort (IQIC) program with the University of Washington Center for Stewardship in Medicine (CSiM) and University of Utah that included 3 types of longitudinal interventions aimed at reducing treatment of ASB: 1) educational sessions, 2) individualized coaching, and 3) data-driven performance feedback reports based on the NQF measure. To create the performance reports, hospitals were asked to submit deidentified clinical and treatment data via a REDCap tool on a random sample of 5-6 adult patients monthly who had a positive urine culture, received antibiotics to treat a UTI, and were admitted or discharged from the emergency department. Bi-monthly performance reports were created from these data to benchmark progress over time and compare ASB treatment to peers. Reports also included treatment duration and empiric/discharge antibiotic use, although these outcomes were not specifically targeted in the intervention. To assess the efficacy of the IQIC program over time, we assessed change in inappropriate diagnosis of UTI (using a mixed-effects logistic regression model). Because we did not intervene on antibiotic duration or avoidable fluoroquinolone use (i.e., fluoroquinolone use in patient without fever, pyelonephritis, or sepsis), we considered these outcomes to be non-equivalent dependent variables and their change over time was assessed (using mixed-effects logistic/linear regression models, as appropriate) as a concurrent control to address confounding by time.
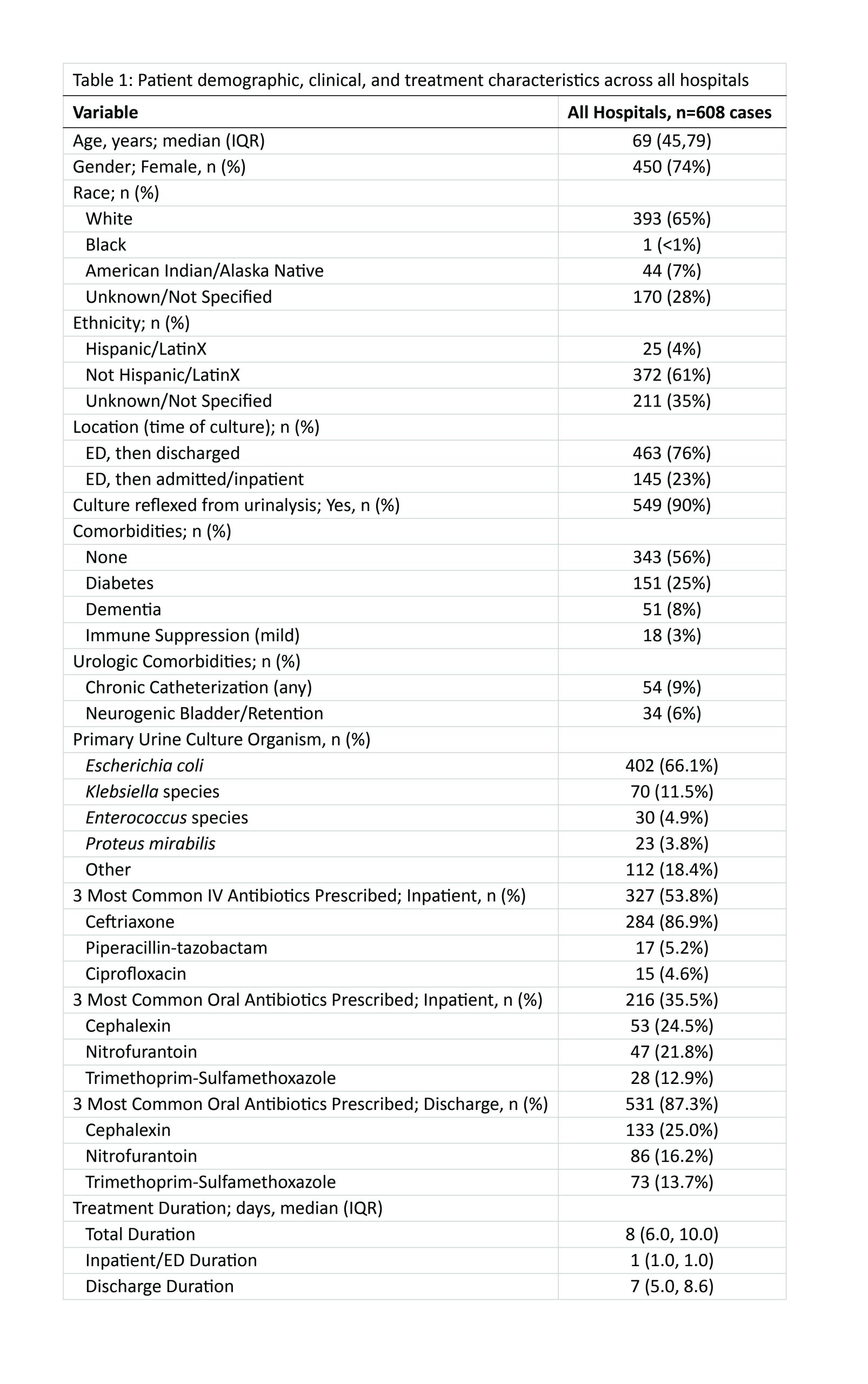
Results: The 10 hospitals used 7 different electronic health records, and 5/10 (50%) had < 25% effort devoted to stewardship. Four of 10 hospitals (40%) abstracted ≥50 cases (goal); 6/10 (60%) abstracted 22-49 cases for a total of 608 cases. Most patients were seen in the emergency department and discharged (76%) and a majority had no comorbidities (56%; see Table 1 for details). Baseline percentage of treated cases with ASB across hospitals was 28.4% (range, 0%-63%). Over the course of the program, the mean percentage of cases treated for UTI that were ASB decreased to 18.6% (range, 0%-33%), a relative decrease of 34.5% (p=0.055). In contrast, antibiotic duration and avoidable fluoroquinolone use remained unchanged (p=0.768 and 0.567, respectively, Figure 1).
Conclusions: The IQIC intervention, including education, coaching, and performance feedback on ASB, reduced treatment of ASB by 34.5%, while control outcomes (duration and avoidable fluoroquinolone use) were unchanged. Despite barriers, critical access hospitals were able to collect sufficient data to measure ASB treatment and use these data to drive improvement.