Background: Up to 50% of the American healthcare spending is estimated to be wasteful. The largest type of wasteful spending is on overuse of tests and treatments. Among the diagnostic tests that are overused, excessive phlebotomy stands out due to its multifaceted implications, including hospital-acquired anemia, patient discomfort, provider burden, and avoidable downstream testing. The imperative to deliver high-value care necessitates the implementation of strategies to curtail unnecessary laboratory testing.
Purpose: This study focuses on a three-phase intervention targeting the overuse of phlebotomy at University Hospital (UH) in San Antonio, TX.
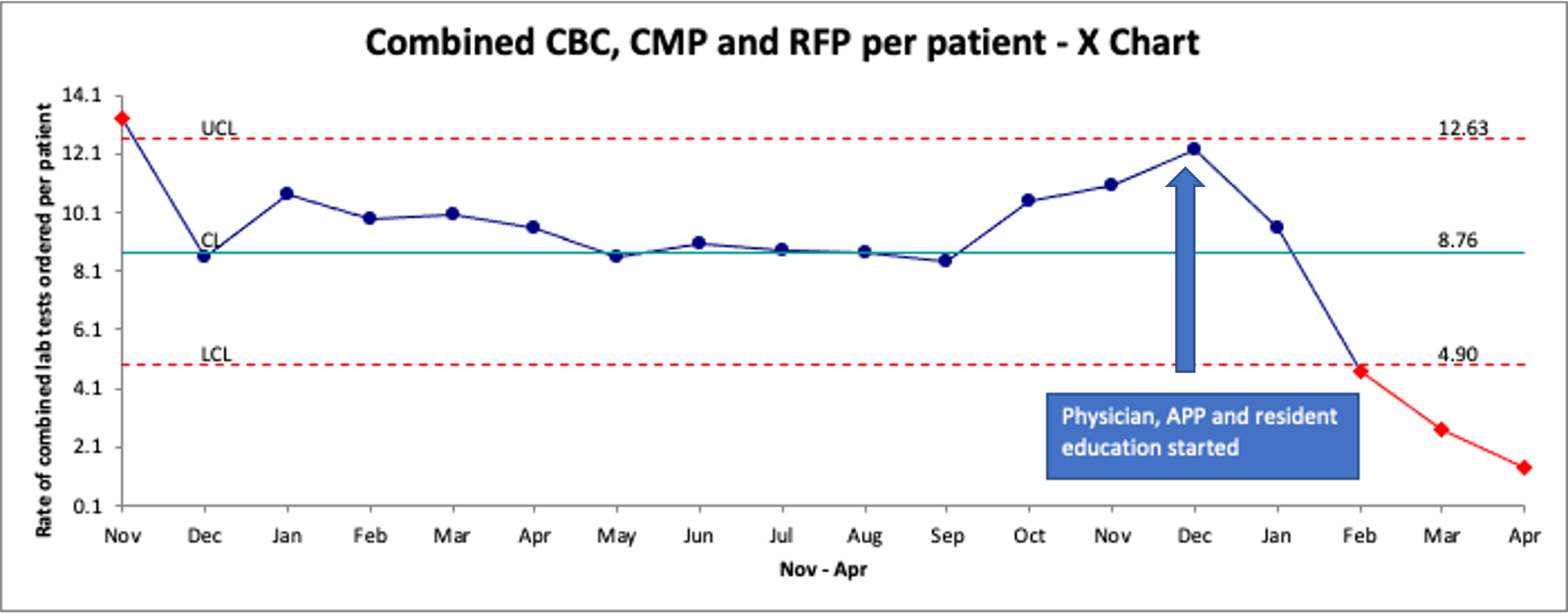
Description: UH is a 700-bed level 1 trauma center that serves as the only academic medical center and county hospital in the area. We have 5 house-staff and 11 direct care teams with an average daily census of 210 patients. Our process improvement project was launched in December 2022 and is divided into three phases: 1. Educational Sessions 2. Provider Feedback, and 3. Electronic Health Record (EHR) based tactics. In phase 1, educational sessions consisting of a didactic slideshow and interactive Q&A segments addressing potential barriers and hesitations to change were conducted. These sessions were conducted twice with the hospital medicine physicians and advanced practice providers, once with internal medicine residents, and once with nursing supervisors, who cascaded the information to their staff. In phase 2, monthly provider feedback packets showing individual provider laboratory utilization rates compared to average utilization rates for the hospital medicine group started going out in August 2023. In phase 3, a hard stop will be introduced in the EHR limiting the ability of providers to order daily laboratory tests for more than 48 hours at a time. We collected the total number of laboratory tests ordered by hospital medicine teams between November 2021 and April 2023. Statistical Process Control (SPC) Charts were employed to visualize the ratio of labs ordered per patient for Complete Blood Count (CBC), Basic Metabolic Panel/Comprehensive Metabolic Panel (BMP/CMP), Renal Function Panel (RFP), and the aggregate of these tests.
Conclusions: SPC chart demonstrates a trend towards reduction in laboratory test utilization after implementation of educational sessions. Aggregate test utilization declined by 37.4%. The utilization of CBC, BMP/CMP and RFP declined 41.2%, 35.9% and 27.1%, respectively. The total cost savings as a result of decreased laboratory test utilization were estimated at $6,310 per month. Education is a key component of Quality Improvement initiatives, empowering healthcare providers to pursue exceptional patient care. While our educational efforts yielded positive outcomes, it is acknowledged that sustaining these results through education alone is resource-intensive, involving instructor preparation, time investment, and ongoing training. Therefore, we have started phase two of our intervention with provider feedback packets that were started in August 2023. We are actively engaged in introducing a hospital-wide hard stop within the Epic EHR, limiting continuous daily lab orders to a 48-hour timeframe.