Background: Although the history of refeeding syndrome is long, few studies provide scientific information regarding refeeding syndrome in frail medical inpatients. In this study, we aimed to investigate the incidence, risk factors, and clinical implications of refeeding syndrome in frail hospitalized patients for acute medical problems.
Methods: This was a single-center retrospective cohort study. Clinical data of patients aged between 20 and 90 years who were discharged alive from the hospitalist-operated acute medical unit at a tertiary hospital were collected. A clinical frailty scale (CFS) score of ≥ 5 indicated frailty, and refeeding syndrome was a decrease of 10% or more in serum phosphorus or potassium within 5 days of admission in patients who admitted decreased oral intake before hospitalization or who received parenteral nutrition after admission. The risk factors for refeeding syndrome were identified by logistic regression analysis. The clinical outcomes were compared according to the occurrence of refeeding syndrome.
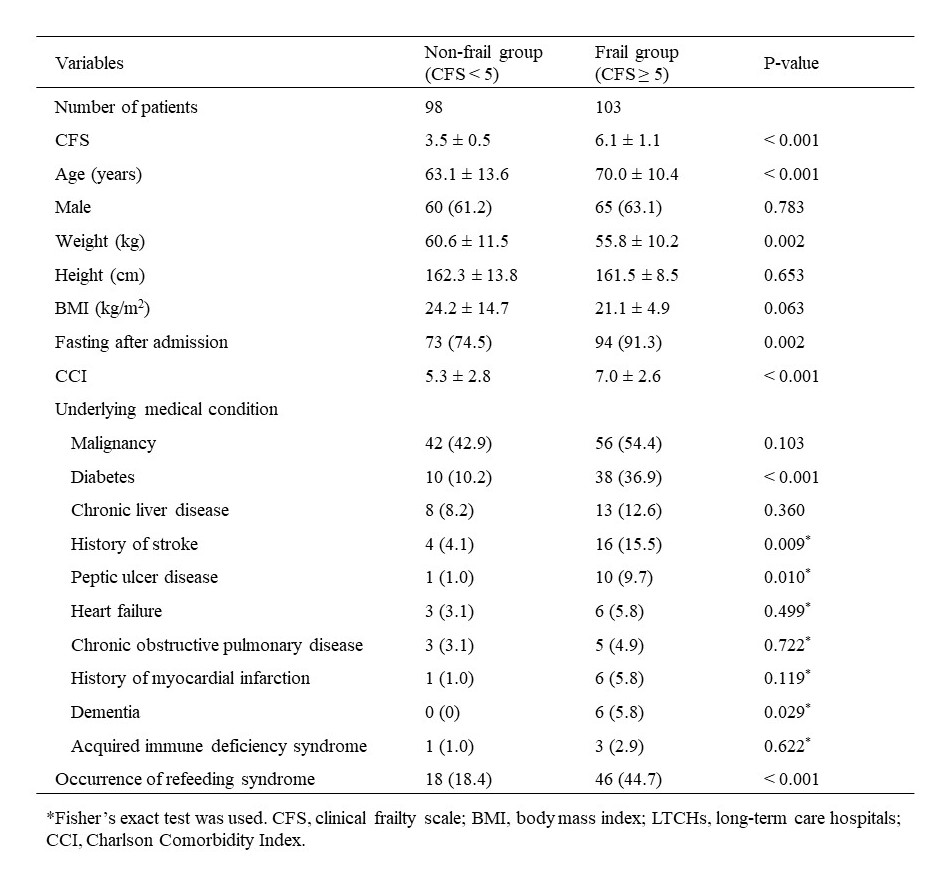
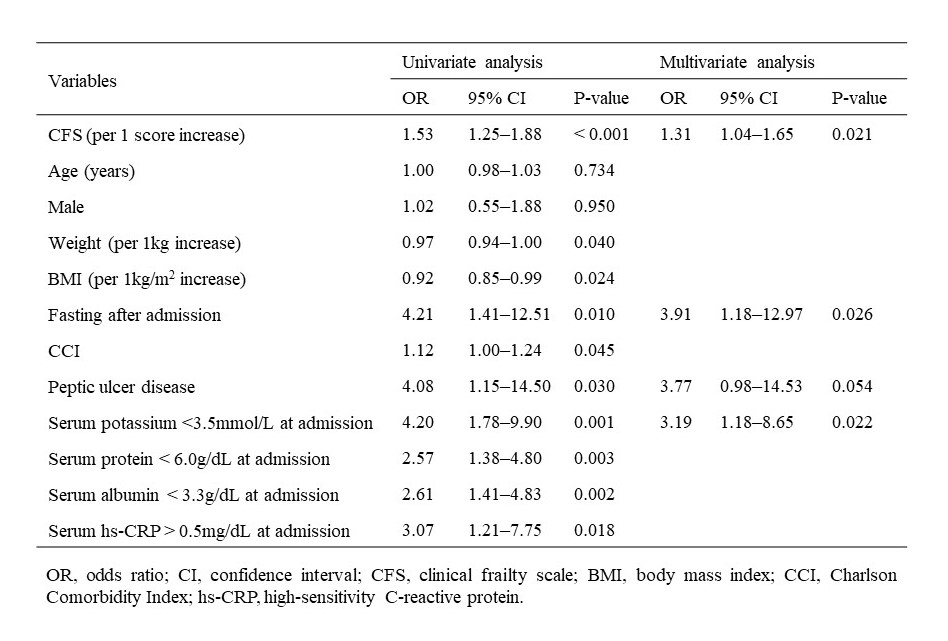
Results: Of the total 201 patients, 103 patients with CFS of 5 or higher were classified as the frail group, and 98 patients with CFS less than 5 were classified as the non-frail group. The frail group was significantly older (70.0 years vs. 63.1 years, p < 0.001) and had a lower body weight (55.8 kg vs. 60.6 kg, p = 0.002) compared to the non-frail group. More patients in the frail group fasted after admission (91.3% vs. 74.5%, p = 0.002), and the mean CCI was also higher in the frail group than in the non-frail group (7.0 vs. 5.2, p < 0.001). The proportions of patients with diabetes, a history of stroke, peptic ulcer disease, and dementia were higher in the frail group than in the non-frail group. Among 103 patients in the frail group, 46 patients (44.7%) had refeeding syndrome, whereas 18 of 99 patients (18.4%) in the non-frail group had refeeding syndrome (p < 0.001). In univariate logistic regression analyses, CFS, weight, BMI, fasting after admission, CCI, peptic ulcer disease, hypokalemia, hypoproteinemia, hypoalbuminemia, and elevated hs-CRP levels showed significant association with the occurrence of refeeding syndrome. After adjustment for significant variables in univariate analyses, CFS (per 1 score increase) (odds ratio (OR): 1.31, 95% confidence interval (CI): 1.04–1.65, p = 0.021), hypokalemia at admission (OR: 3.19, 95% CI: 1.18–7 = 8.65, p = 0.022), and fasting after admission (OR: 3.91, 95% CI: 1.18–12.97, p = 0.026) were independent risk factors for refeeding syndrome. When comparing clinical results according to the presence or absence of refeeding syndrome, patients with refeeding syndrome showed a significantly longer hospital stay (mean, 21.5 vs. 14.2 nights, p = 0.018) and more pressure ulcers (15.6% vs. 3.6%, p = 0.003).
Conclusions: Refeeding syndrome, which was shown to be significantly associated with clinical outcomes such as length of hospitals stay and pressure ulcer, occurred frequently in frail patients. High CFS, which is indicative of frailty, was found to be a risk factor for the development of refeeding syndrome.