Background: Millions of patients are discharged to skilled nursing facilities (SNFs) each year. In teaching hospitals, resident physicians are often responsible for organizing this transition. Understanding residents’ knowledge and experiences of this care transition has the potential to inform residency training, education, and clinical experience. This study aimed to explore residents’ attitudes and experiences in discharging patients to SNFs and identify perceived challenges to this common process.
Methods: We conducted a qualitative study using focus groups within one internal medicine and one surgical residency program. These programs’ residents worked at three urban hospital sites (a tertiary academic center, a county hospital, and a Veterans Affairs medical center). A focus group guide was developed containing seven questions exploring residents’ experiences and knowledge around discharging patients to SNFs. Separate focus groups were conducted for medicine and surgery residents. Focus group data were analyzed using thematic analysis.
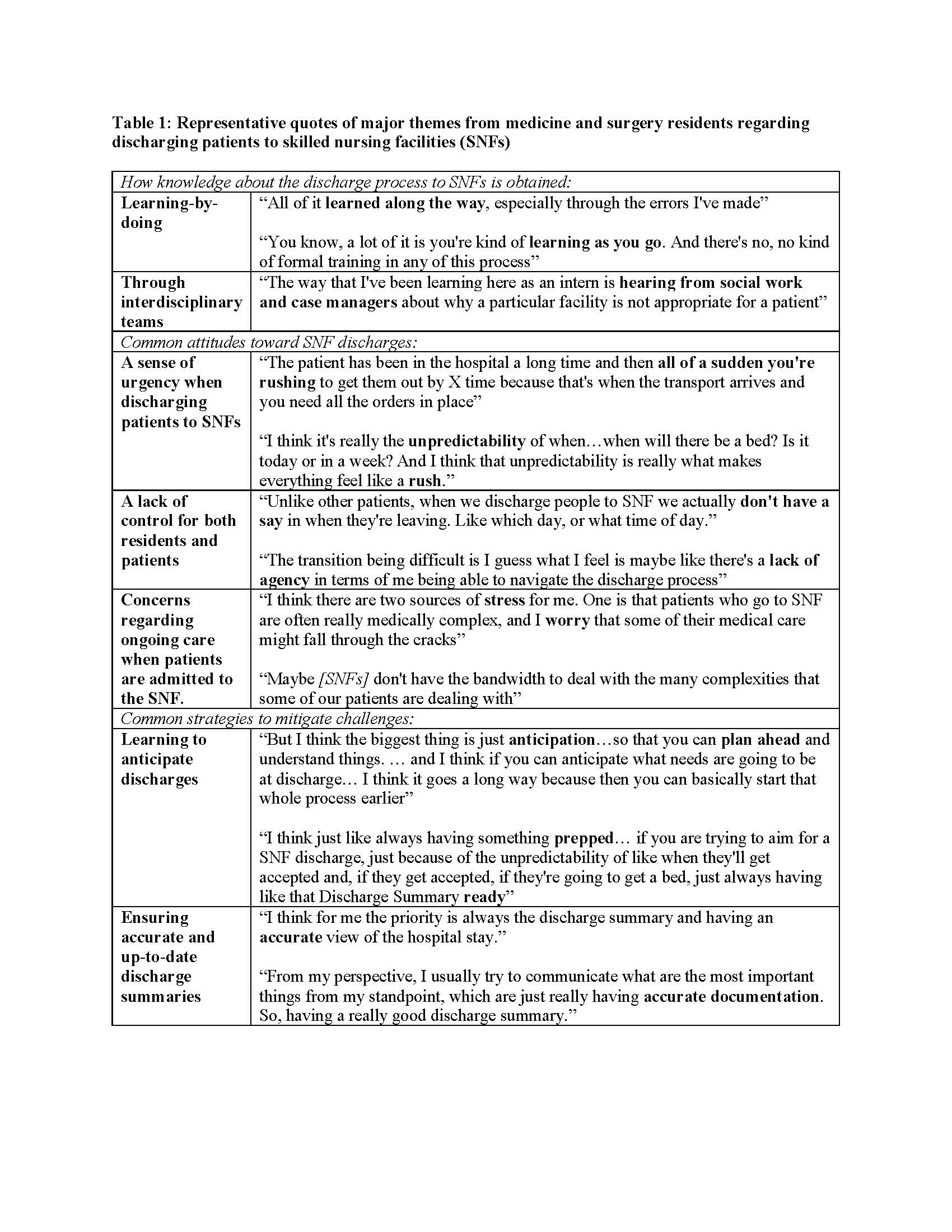
Results: We recruited 20 residents (n=10 medicine, n=10 surgery) interviewed in 6 focus groups. Regardless of specialty, residents had similar experiences of this transition of care. Prior education and clinical exposures to SNFs were uncommon. Most residents learned about the services that SNFs provide indirectly: through patients, interdisciplinary team members (e.g., case managers), or the media. Few residents had stepped foot inside of a SNF. Most residents endorsed that their knowledge around the process of discharging patients to SNF was obtained through “learning by doing”. The most common attitudes from residents about discharging patients to SNFs were 1) a sense of urgency, 2) a sense of lack of control, for both residents and patients, and 3) concerns regarding ongoing care for patients who were admitted to SNFs. Residents endorsed that they try to mitigate these challenges by focusing on aspects of the discharge to SNF that they can control, specifically by 1) learning to anticipate discharges and 2) ensuring accurate and up-to-date discharge summaries to highlight priorities and tasks for SNF clinicians. Surgical residents noted that over time, advanced practice providers (APPs) were completing more key elements of organizing discharges to SNFs. In contrast, this programs’ internal medicine residents did not work with APPs. Representative quotes related to key themes are shown in Table 1.
Conclusions: Medicine and surgery residents described a lack of formal education and clinical exposure to SNFs. These findings align with other research describing other clinicians lack of knowledge about SNFs. The lack of education and knowledge may be contributing to residents’ attitudes of uncertainty, sense of lack of control during discharge planning, and concern for the quality of care received by patients. These results suggest that residency programs should adopt formal clinical curriculum and rotations on or at SNFs.