Background: First year hospitalists have higher inpatient and 30 day post discharge mortality than hospitalists with at least a year of experience. The Joint Commission found that improper orientation and training is the second leading cause of sentinel events in hospitals. There is neither literature nor guidelines to inform best practices for Hospital Medicine (HM) onboarding. With many HM programs understaffed, hospitalists are often pressed into action.
Purpose: We sought to re-engineer our new physician onboarding program to emphasize patient safety and quality as well as physician wellness.
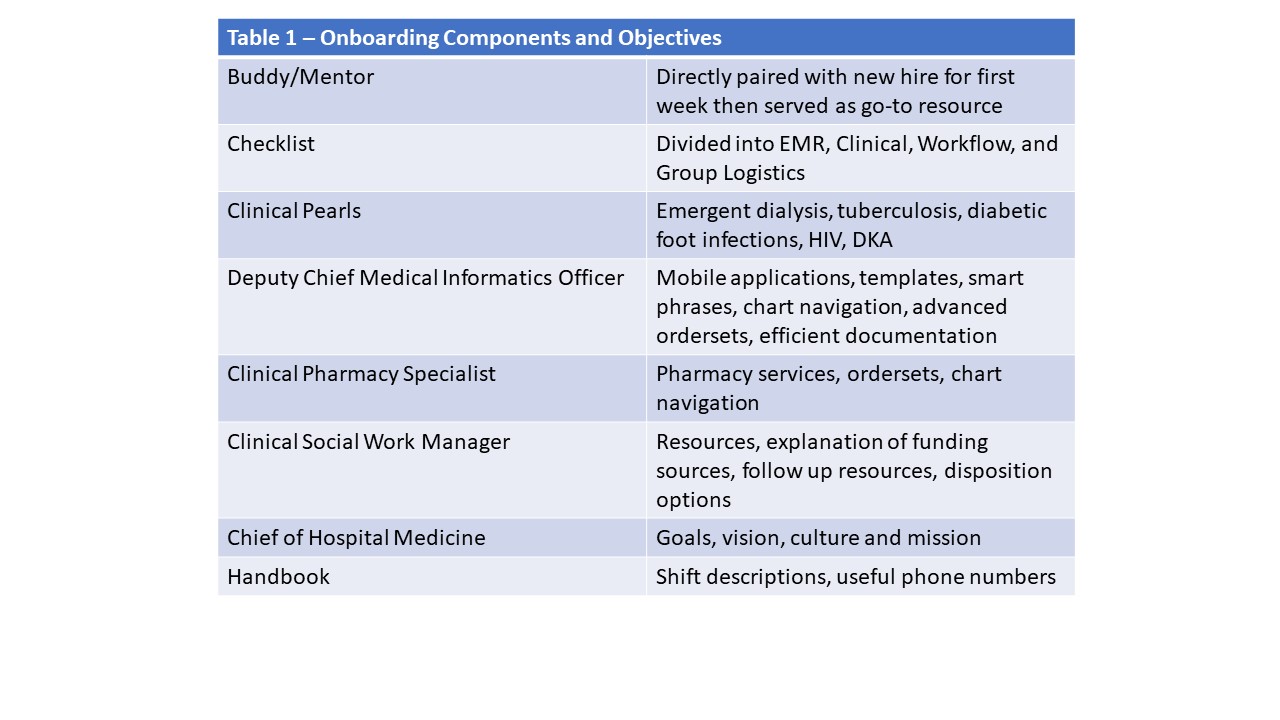
Description: The components of our new onboarding program are as in Table 1.
On their first day, the Medical Director of Faculty development met with the new hire and mentor to go over the checklist, clinical pearls document and the overall program. The Deputy Chief Medical Informatics Officer (a hospitalist), a clinical pharmacy specialist, a social work manager and the Chief of HM met with each new physician in their first two weeks (Table 1).
Each new physician also received a HM specific handbook and a welcome gift basket.
Work load was gradually increased. During the 1st week, the new physician was paired with his/her mentor and would see 2 patients the 1st day increasing to 8 by day 7. The 1st week practicing independently was capped at 8 patients daily then 10 daily the 2nd week then 11 daily the 3rd week and 12 patients daily the 4th week. Starting the 5th week (month 3), the physician would see the same number of patients (13-14) as others.
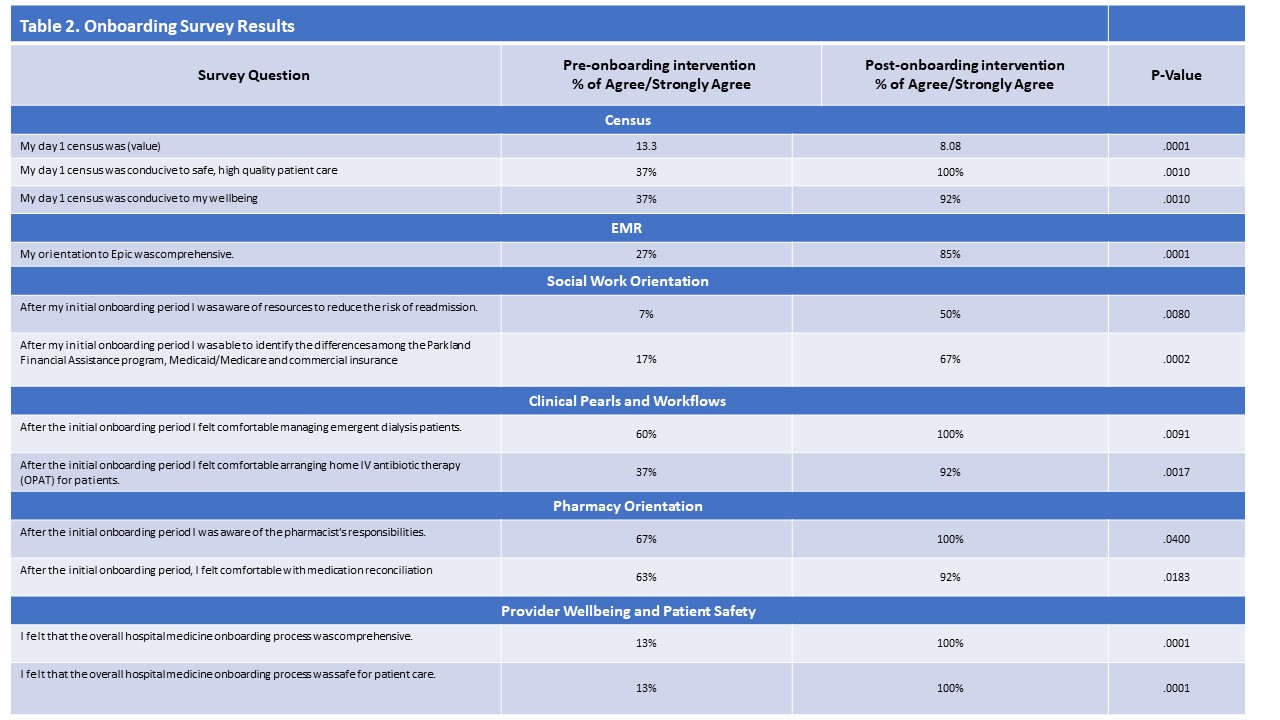
From July –October of 2018, 15 new faculty started and experienced the new onboarding program. 13 of the 15 had just finished residency. We surveyed both new and prior faculty to determine their perceptions of how their onboarding affected patient safety and their well-being. 12 of the 15 (80%) new physicians responded and 30 of the 46 (65%) of previously onboarded faculty responded for an overall response rate of 69% (42/61)
When compared to previously onboarding faculty, our new faculty felt that the new process was comprehensive (13% v 100% p<0.05) and both conducive to physician wellbeing (37% v 92%, p<0.05) and safe, high quality patient care (37% v 100%, p<0.05). Table 2.
Conclusions: We redesigned our new physician onboarding program to prioritize patient safety and physician well-being. The program was well received by new physicians and prior physicians alike. Further investigation as to the downstream effects (quality indicators, patient satisfaction, retention) of the new onboarding program are indicated.