Background: The use of contact precautions (CP) for patients with colonized or infected (endemic) methicillin-resistant staphylococcus aureus (MRSA) is common in many hospitals, but emerging literature does not support CP over standard precautions in preventing hospital acquired infection. CP use has been associated with delays in admission and discharge, fewer bedside evaluations, preventable adverse events such as falls and pressure ulcers, as well as depression and anxiety in patients, and decreased patient and provider satisfaction. Given the lack of proven benefit and potential harms, several hospitals have reevaluated their policies related to CP. Within our health system, two large community hospitals piloted a program that eliminates the use of contact precautions for historical MRSA. In preparation for similar plans at our large academic center, we developed a survey to identify the attitudes, perceptions and knowledge of CP
Methods: We compared National Healthcare Safety Network (NHSN) LabID rates one year before and after discontinuation of personal protective equipment (PPE) at two community hospitals that discontinued CP for historical MRSA. We developed a survey exploring knowledge and perceptions of internal medicine residents at our institution. Survey items asked the degree to which residents agreed with potential risks and benefits of contact precautions utilizing a Likert scale. The survey was anonymous and voluntary.
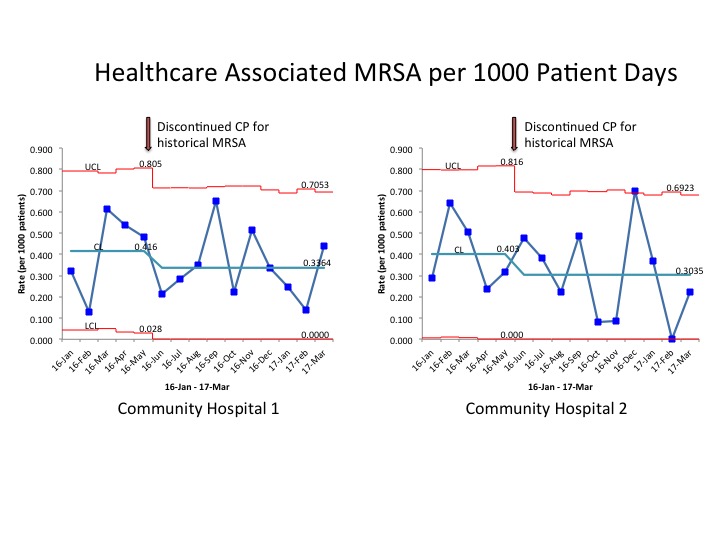
Results: There was no difference between NHSN LabID rates in the year preceding and following discontinuation of CP for historical MRSA in two community hospitals within our health system. Analysis using statistical process control charts demonstrated no change in healthcare associated MRSA infections per 1000 patient days.
Forty-four residents completed the survey. Of those, 23 (52%) reported spending less time in CP rooms, 19 (43%) entered CP rooms less frequently, and 28 (64%) were unfamiliar with policies delineating when CP may be discontinued. Residents perceived an increase in hospital-associated anxiety or depression in patients under their care (84%), patient falls (63%), pressure sores (59%) and medication errors (57%). Thirty (68%) perceived that CP was associated with a decrease in patient satisfaction. Twenty-three residents misperceived that entering rooms only briefly does not require CP and 19 residents reported donning CP is time consuming.
Conclusions: The results are consistent with the emerging body of literature that demonstrates no change in MRSA rates with the discontinuation of CP. Our residents accurately perceived the potential harms of CP and therefore, may serve an important role in education as we design and implement a plan for discontinuation of CP in our institution. The survey results will be used to guide current and future policies pertaining to CP within our academic medical center.