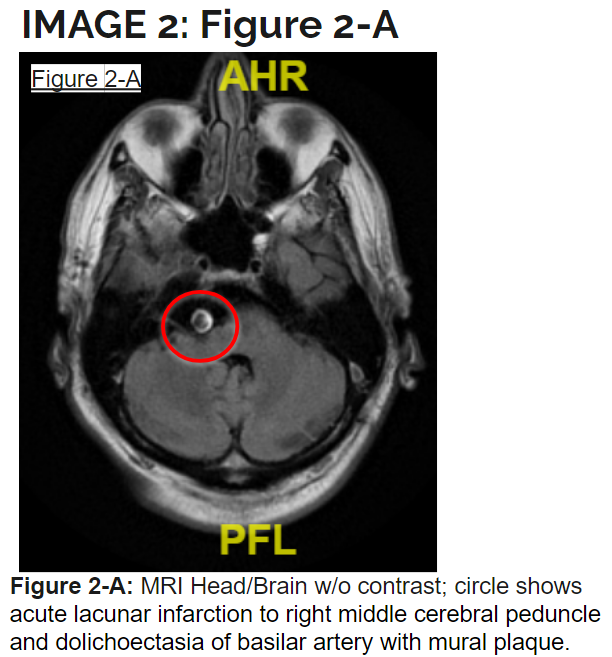
Case Presentation: Dolichoectasia is a rare disorder of the cerebral arteries known to causes tortuosity, elongation, and dilation of the affected vessel. Most commonly involved vessels are those of the vertebrobasilar circulation, with an elevated risk of ischemic infarct. Here we have a case of such a rare presentation of ischemic stroke in the setting of dolichoectasia causing recurrent infarcts with the most recent insult affecting the right middle cerebral peduncle. 63-year-old male presented to the emergency department with complaint of acute onset of left-sided numbness and weakness, along with tinnitus, diplopia, slurred speech and headache. On examination he was found to have dysmetria of his bilateral upper extremities and left lower extremity as well as dysarthria. History revealed that patient had developed an ischemic CVA three-weeks prior with right-sided deficits in addition to an ischemic CVA four-months prior with left-sided deficits, however deficits had resolved since these insults. After his first CVA four-months prior, he was informed of an abnormal artery in his brain. Currently being treated with Clopidogrel 75 mg, Aspirin 81mg and Atorvastatin 81 mg daily. His blood pressure medications were stopped, excepted for Losartan 12.5 mg with the goal of keeping his blood pressure elevated.
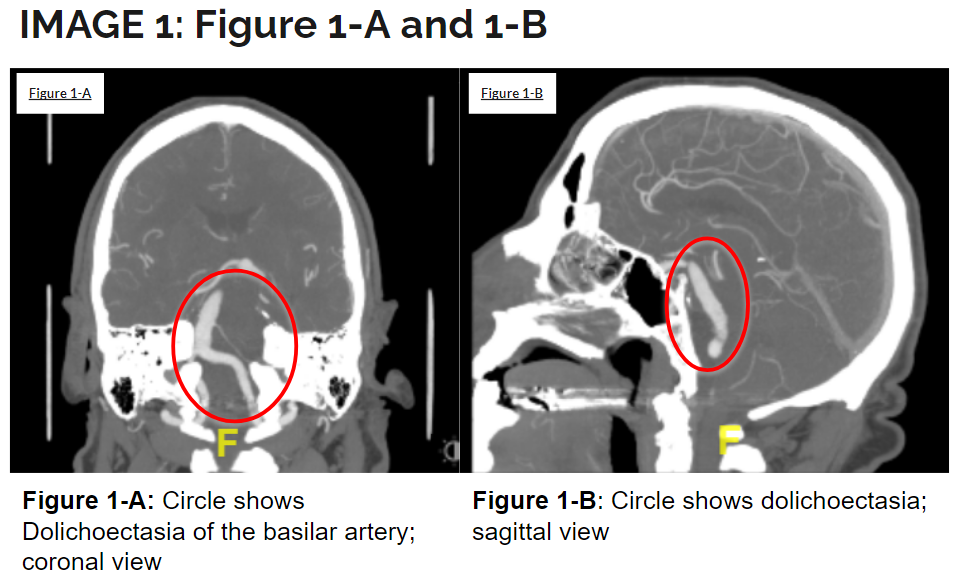
Discussion: CT head and brain without contrast showed prominence of the basilar artery measuring up to 10 mm in diameter. CT angiography head and neck showed dolichoectasia of the basilar artery with fusiform ectasia without saccular aneurysm formation, and mild tortuosity. MRI head brain without contrast demonstrated an acute lacunar infarction in the right middle cerebral peduncle with dolichoectasia of the basilar artery with mural plaque. He was not a surgical candidate for stenting given basilar artery diameter. Compassionate use of basilar artery flow diversion in the future if recurrent Posterior Circulation Strokes were to occur was discussed. Medical management to control patients underlying risk factors was targeted. Atorvastatin 80 mg was continued. Following the window for permissive hypertension the decision was made to target a goal blood pressure of 140s/90s with the addition of Carvedilol 12.5mg twice daily and increasing home Losartan to 50mg daily. Platelet Reactivity Units (PRU) was measured at 195. In addition, Apixaban was added to augment his antiplatelet therapy and reduce thromboembolic events. He was evaluated by physical, occupational and speech therapy. At discharge he was sent to in-patient rehab for aggressive rehabilitation with noticeable improvement of his left-sided functionality.
Conclusions: Our patient presented with repeated stroke with most recent infarcts occurring 3 weeks apart, and unfortunately in the setting of dolichoectasia he faces increased mortality risk. Given his dilated basilar artery of approximately 10 mm, he was not a candidate for potential stenting. Blood pressure management included maintaining a maximum blood pressure of 140/90 contrary to what he was previously recommended. In addition, Apixaban 5 mg twice daily was added to his current Clopidogrel 75 mg daily regimen and Aspirin 81mg daily was stopped. Its important to recognize that Dolichoectasia, the rare disease that it is, currently has no proven guideline treatments as of yet and management for supportive treatment strategies should continue to be investigated. This case report serves to aid other physicians whom may encounter such a remarkable presentation of an acute ischemic stroke.