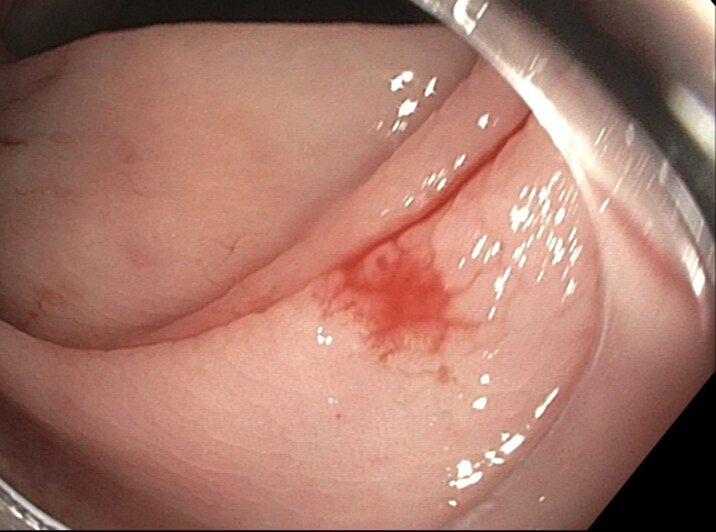
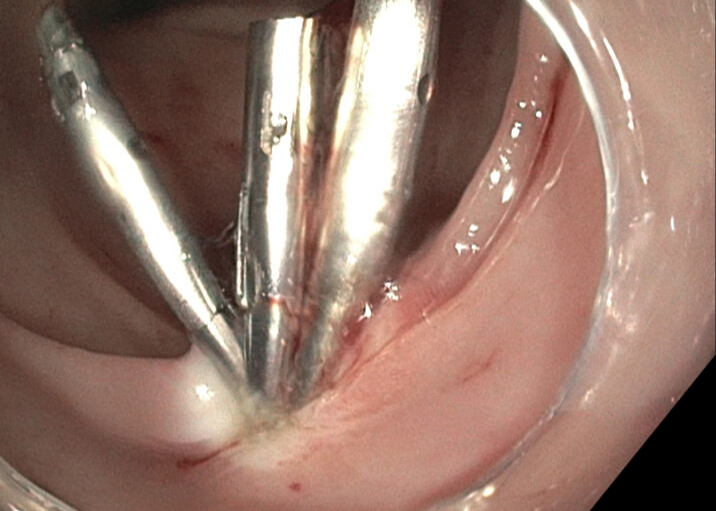
Case Presentation: The patient is a 51 year old male with diabetes, peripheral arterial disease with extensive vascular surgeries including left below the knee amputation, ESRD on hemodialysis, multivessel coronary artery disease, history of seizures, who presented with altered mental status likely from missed dialysis. Patient was found to be afebrile, hypertensive to the 200s systolic, and saturating well on room air. GCS was 9 and admission labs were notable for Cr 11.45, BUN 93, AG 25.5, HCO3 21, WBC 7.5, and Hgb 8.4 Following multiple sessions of dialysis, the patient began to have large, dark bloody bowel movements requiring multiple blood transfusions. Colonoscopy was performed and showed large amounts of blood but no definite source of the bleeding. Following the colonoscopy, he had an esophagogastroduodenoscopy (EGD) which noted normal esophagus, stomach, and duodenum. PillCam capsule was then performed, but unfortunately, the source of the bleed still could not be localized. Subsequently, a tagged RBC study was conducted, yielding abnormal tracer activity ectopic to blood pool, suggesting active GI bleed in the right upper quadrant, in the region of the hepatic flexure . To target this area, an IR embolization attempt was made which yielded no angiographic evidence of a bleed. This unsuccessful embolization attempt was followed by a repeat, unsuccessful colonoscopy. Ultimately, a large bowel capsule was completed which showed an oozing AVM (Figure 1) in the ascending colon, which was deemed the likely source of bleeding. Three hemoclip placements were made, however, given continued bleeding despite the clips, a hot snare was utilized over the clips for hemostasis (Figure 2). Following this capsule procedure, the patient’s bowel movements became non bloody, and hemoglobin stabilized, not requiring additional transfusions. In total, 23 units of blood were transfused over an approximate 1 month stay.
Discussion: AVMs are not uncommon findings in patients presenting with GI bleeds. However, those with ESRD are more prone to develop angiodysplasia and malformations (1) and thus are at high risk of developing an acute GI bleed. Our report demonstrates a unique case of how elusive these malformations may be. The technical difficulty of colonoscopy cannot be understated. There are difficulties in ensuring patients have adequate bowel prep as well as reaching anatomically challenging regions such as the sigmoid colon and the hepatic flexure. In patients with ESRD, achieving hemostasis also presents a challenge due to platelet dysfunction. While most AVMs may be dealt with using only hemoclips, our case also demonstrates a successful concomitant use of hot snare with hemoclips. Despite the risks of thermal injury and delayed rebleeding, this technique may be an option in patients with difficult bleeds.
Conclusions: Our report demonstrates not only the technical challenges, but also the complexity involved in a patient with multiple comorbidities that required extensive interventions to stop a GI bleed. Patients may require multiple scopes and pill endoscopy. Once bleeding is localized, hot snares may be utilized in conjunction with hemoclips to achieve hemostasis.