Background:
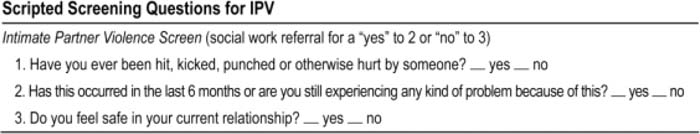
Although numerous professional organizations recommend routine screening for intimate partner violence (IPV), and the Joint Commission for Accreditation for Health Care Organizations requires screening for IPV in in patient admissions, screening rates in outpatient and inpatient settings remain low. Barriers to screening for IPV include uncertainty about how to elicit this information, uncertainty about how to proceed when a woman discloses IPV and belief that effective interventions are lacking. Interventions designed to increase screening for IPV in the outpatient setting yield modest results, and no study has looked at increasing screening lor IPV in the inpatient setting. The objective of this study was to increase screening rates for IPV on an inpatient medicine teaching service by providing scripted screening questions and a prompt about how to proceed with a positive screen.
Methods:
This study was approved by the Colorado Multiple Institution Review Board with waiver of informed consent. Women between the ages of 18 and 60 admitted to a medicine inpatient service by a resident at a university‐affiliated public safetynet hospital were included. We prospectively determined IPV screening rates after revising the social history section of our standard history and physical template to include scripted questions to screen for IPV and a prompt about how to proceed for positive responses. We compared this with a previous study performed in our medicine inpatients that revealed a resident screening rate for IPV of 25%.
Results:
From July 31 to October 14, 2008, the study history and physical template was completed for 208 eligible women, and 82 of those were screened for IPV using the screening questions (39.4%). This was a 56% increase in screening rates compared to the baseline of 25% (P < 0.05). Thirteen of the 82 women (16%) reported histories of IPV within the 6 months prior to their hospitalization. Of these, only 7 (54%) were appropriately referred to a social worker. Patients seen by a social worker received resource information and help with safety planning, and 2 of the 7 women (29%) referred to a social worker left their abusive relationship directly from the hospitalization.
Conclusions:
Although providing scripted screening questions on a history and physical template increases screening rates for IPV in women admitted to medicine teaching services, the increase is modest. These results suggest that the inpalienl setting is a viable place for interventions for those with histories of IPV, however, adding a prompt for a social worker referral does not ensure that patients are appropriately referred. Additional studies are needed to further increase screening rates and interventions for IPV in the inpatient setting.
Author Disclosure:
B. Cleary, none; A. Keniston, none; R. Albert, none.