Background: Telemetry beyond 48 hours is indicated for a select patient population and when used inappropriately has risk. This includes increased cost of care, skin irritation, delirium contribution, and more likely to have false positives resulting in errors or extending length of stay.To encourage care that is truly necessary, free of harm, not duplicative, and evidence-based Society of Hospital Medicine through the Choosing Wisely campaign recommends “Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.”In a large hospital, the hospitalist quality committee identified opportunity to decrease telemetry duration.
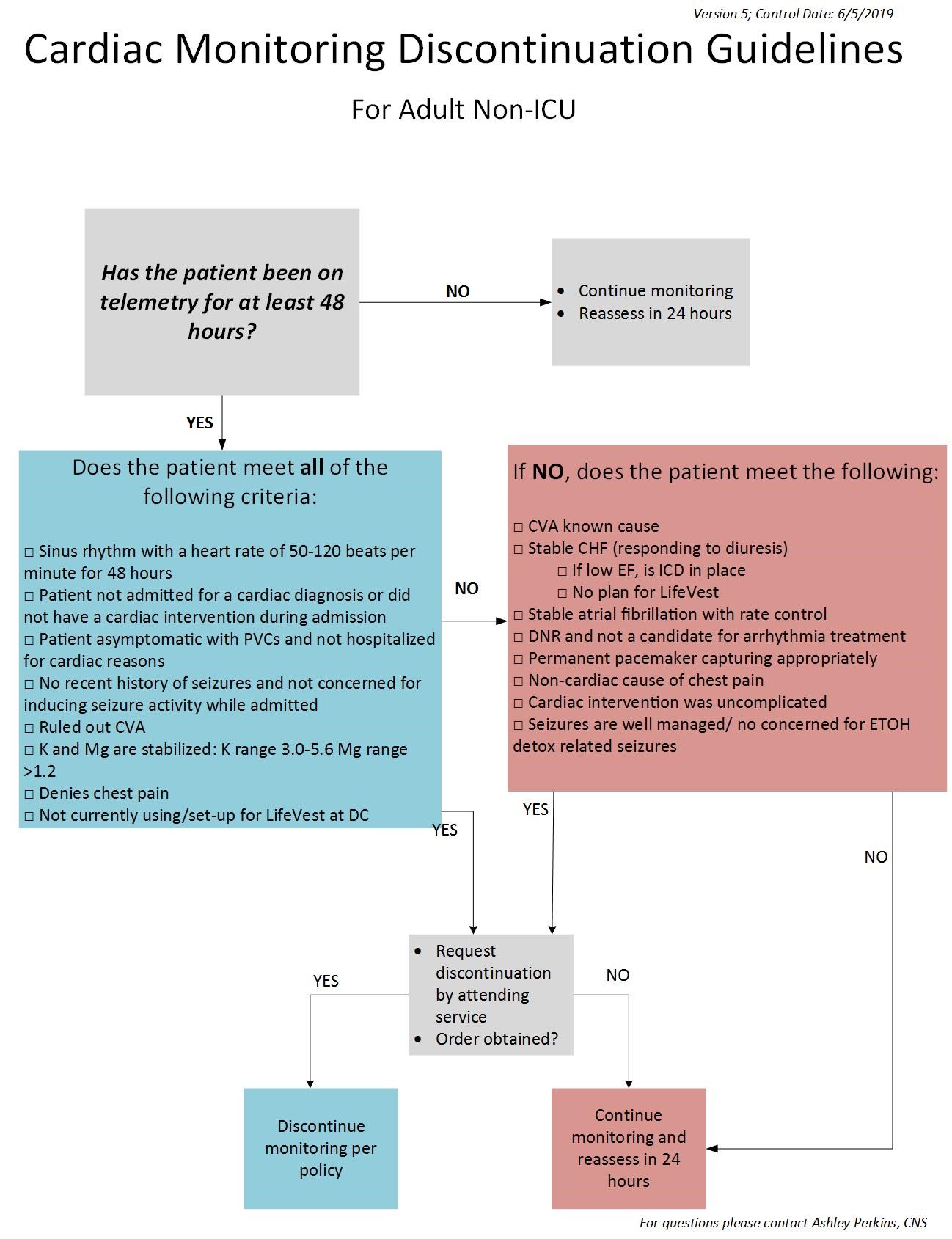
Methods: Institution IRB approval designated project a non-human research exemption. Based on 2017 AHA guidelines for duration of cardiac monitoring, an algorithm (figure 1) and standard activity were developed. 6 floors were chosen to participate. Criteria was interdisciplinary rounds (I-Rounds) with a hospitalist physician, unit secretary to identify reports of patients on telemetry greater than 48 hours, and a nurse manager available to monitor standard work.Educational sessions were held with hospitalist providers. Focus was on the benefit of removing telemetry when no longer necessary, indications of placing telemetry, and awareness that nurses will be reviewing this algorithm and discussing during I-Rounds.Testing period occurred Jan- Mar 2019. Unit secretaries alerted the bedside nurse of patients on telemetry more than 48 hours. The nurse used the algorithm to determine if patient may be considered to discontinue telemetry. This determination was discussed with the provider and order placed when appropriate.Additionally, posters about indication for cardiac monitoring were placed in work spaces. A physician champion provided frequent reminders in multiple formats. Provider patient lists included a column to indicate if cardiac monitoring is in place.
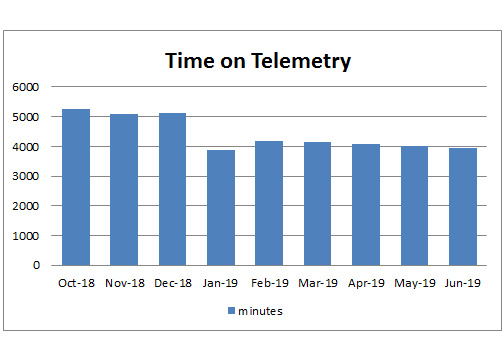
Results: Baseline data on these I-Round units, telemetry duration was 85.9 hours per patient Oct – Dec 2018. Goal to reduce this by 12 hours or to 73.9 hours per patient after intervention.An 18.1 hour reduction per patient (Figure 2) achieved. No serious safety events due to discontinuation of telemetry were reported.An 18.1-hour reduction in telemetry duration equates to $8.33 in savings per patient. During the intervention period, there were 3,018 cardiac monitoring orders. With the 18.1-hour reduction of duration, there was a potential savings of $25,139.94 for the system surpassing $100,000 for the year.
Conclusions: Utilizing a team-based approach, systems can align cardiac monitoring duration to national guidelines improving patient care while reducing waste. Education, algorithm, and standard work successfully decreased duration of telemetry beyond the initial goal. This practice has continued, and these floors sustained lowered telemetry extent (figure 2).Overall duration remains above 48 hours. This may vary by patients with continued indications and prolonged stays. The most positive impact from this project was bridging the care team. Nurses advocated for their patients by using the evidence-based algorithm. Physicians gained heightened awareness of telemetry indications and inappropriate use. Together, they were able to promote high value care that is patient centered, evidence based, data driven, and integrated in provider work flow.