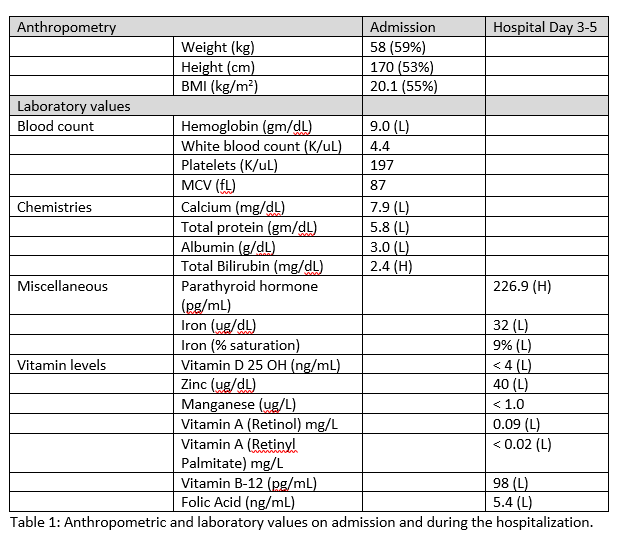
Case Presentation: A 14-year-old male presented to an emergency department with 6 days of left thigh pain and inability to bear weight following a fall from bed. Associated symptoms included nausea, diaphoresis and weakness. Review of systems revealed pallor, easy bruising and yellow eyes. history was negative except for developmental delay, described as auditory processing issues. He had no prior hospitalizations or significant family history. Physical examination showed normal vital signs and growth parameters, poor dentition, mild scleral icterus, pallor and a I/VI systolic ejection murmur. Liver was palpable 2 cm below the costal margin. The left lower extremity (LE) was externally rotated and flexed at the hip. Both LEs had limited range of motion at the hip due to pain. Tenderness to palpation of the left thigh was noted. Exam was otherwise normal. Initial workup revealed normocytic anemia and mild hyperbilirubinemia (Table 1). Left femur, pelvis and bilateral hip x-ray showed bilateral femoral neck fractures and diffuse osteopenia, suggestive of metabolic or infiltrative disorder (Figure 1). MRI Pelvis showed bilateral femoral fractures, abnormal enhancement of hip and thigh muscles, and hip joint synovium. Leading differential at this time included malignancy or infectious process. Further labs demonstrated elevated inflammatory markers, but normal lactate dehydrogenase (LDH), uric acid, peripheral smear, haptoglobin and red blood cell studies. Parathyroid hormone was elevated and vitamin D was low.
During admission, patient’s oral intake was poor, prompting discussion of diet. Mother reported a long history of food refusal; home diet consisted of cola, fish sandwiches and chips. Suspicion for multiple nutritional deficiencies (ND) led to additional labs confirming deficiencies of iron, folic acid, vitamin B12, zinc and vitamin A. Supplemental formula feeds, vitamins and nutritional counseling were started; G-tube was placed. Discharge occurred once feeds were tolerated. Repeat labs at 2 months showed normalization of all labs and vitamin levels.
Discussion: Sensory processing disorders place patients at risk for ND due to an inability to tolerate various tastes and food textures. Diagnosis of one type of sensory disorder should alert clinicians to monitor for other manifestations. Normal growth parameters can mask ND when intake is adequate in calories but not vitamins and minerals, highlighting the importance of obtaining a detailed dietary history. Depletion of multiple nutrients results in a diverse clinical picture, mimicking systemic illness and further confounding diagnosis. A high index of suspicion must be maintained.
Conclusions: Children with sensory disorders are at risk for ND due self-restriction of diet. Consider ND in any child who presents with anemia, unexplained fractures, or hyperbilirubinemia, even in the setting of a normal growth chart.