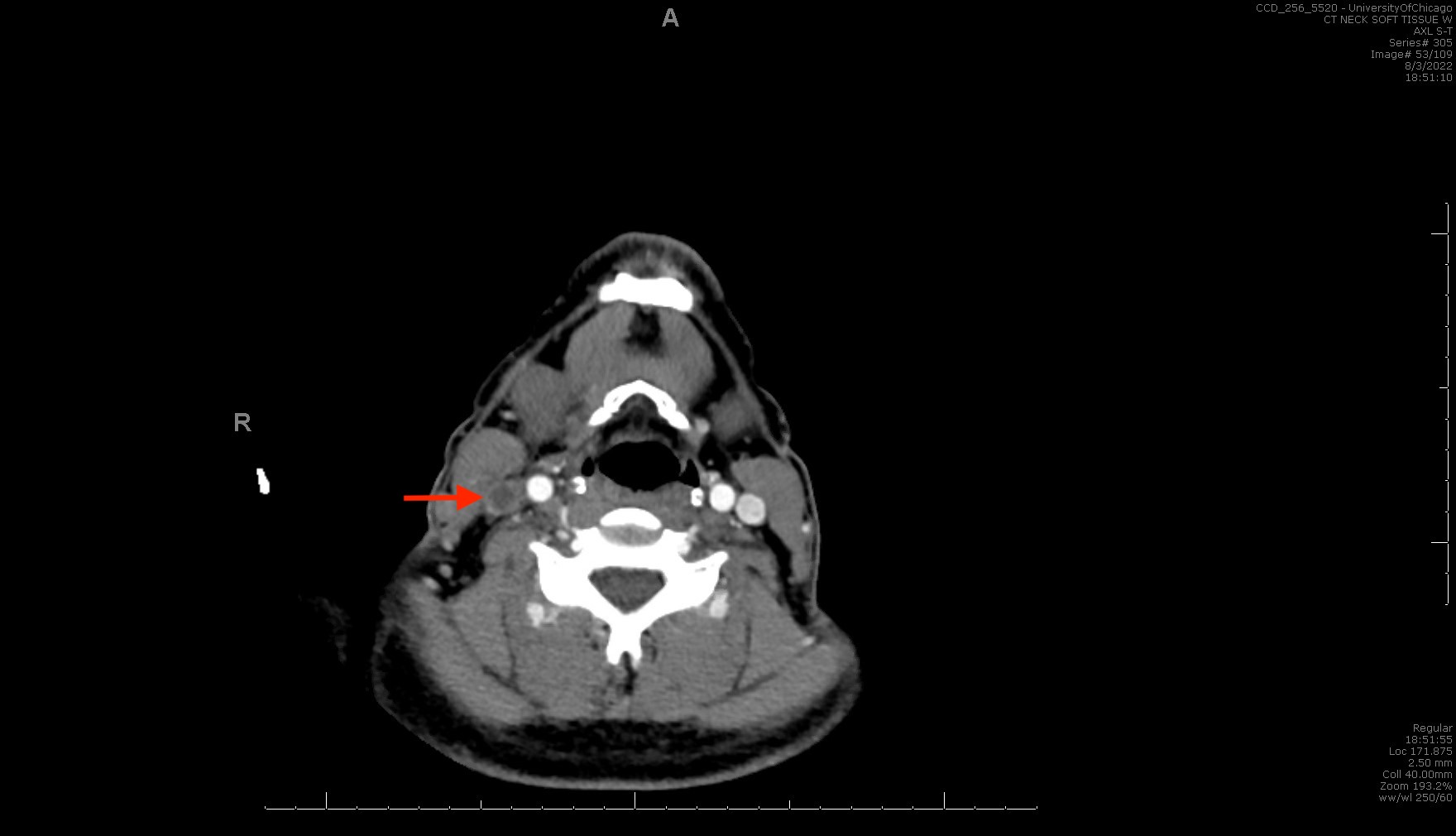
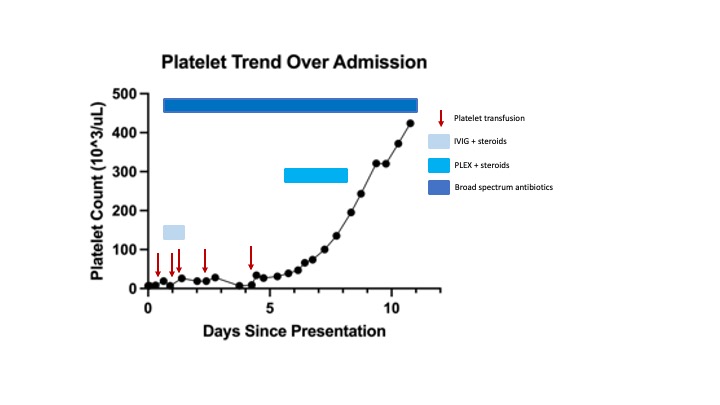
Case Presentation: Lemierre’s syndrome is a clinical syndrome characterized by septic thrombophlebitis of the internal jugular (IJ) vein after an oropharyngeal infection. We present a case of a 36-year-old man with no significant past medical history who presented with one week of subjective fevers/chills, sore throat, and dysphagia. On initial evaluation, vital signs were only notable for tachycardia. Exam revealed cervical tenderness, oropharyngeal exudate, erythema, and peritonsillar swelling. Initial laboratory testing was notable for a white blood cell (WBC) count of 17,600/µL, a hemoglobin of 15.7 g/dL, and a platelet count of 7,000/µL. Imaging of the neck demonstrated extensive inflammation of right-sided deep neck spaces, a partially occlusive thrombus of the right internal jugular vein (Fig. 1), and multiple lung nodules – findings consistent with Lemierre’s Syndrome. The patient was started on ceftriaxone, metronidazole, and vancomycin. Despite platelet transfusions, his thrombocytopenia persisted. Treatment with intravenous immunoglobulins and prednisone was initiated for presumed immune-related thrombocytopenia (ITP). The patient’s condition continued to worsen. Blood cultures grew Fusobaterium necrophorum. He remained afebrile but had a persistently rising WBC count. Antibiotics were changed to Ampicillin+Sulbactam. The patient continued to be severely thrombocytopenic requiring multiple transfusions (Fig. 2). On day 5 of hospitalization, the patient was found to have a hemoglobin of 7.7 g/dL, lactic dehydrogenase 2830 U/L, undetectable haptoglobin, INR 1.6, and schistocytes on his blood smear. These values had been normal on admission. PLASMIC score was 6 and urgent plasma exchange and steroid treatment were initiated for presumed thrombotic thrombocytopenic purpura (TTP). ADAMTS13 level was drawn, and 3 days later it returned showing only a mildly decreased level (57%). Antibiotics were continued for the remainder of the patient’s admission (11 days total) with normalization of platelet count, WBC count, and improvement of anemia. He was discharged home with Ampicillin+Clavulanate for a total of 4 weeks of treatment.
Discussion: Thrombocytopenia associated with Lemierre’s syndrome is increasingly being recognized. However, severe thrombocytopenia and hemolysis are unusual. The etiology of the patient’s severe thrombocytopenia remains elusive. Treatment for presumed ITP did not improve his platelet count. Despite initial concern for TTP and a high PLASMIC score, his ADAMTS13 level returned at a level inconsistent with this. Disseminated intravascular coagulation is a potential etiology however his coagulopathy was mild and disproportionate to his thrombocytopenia. Fusobacterium infections may cause thrombocytopenia through hemagglutinin-induced platelet aggregation. Fusobacterium necrophorum has been shown to have hemolytic activity via production of hemolysin. It possible Lemierre’s syndrome itself caused this patient’s thrombocytopenia and hemolysis through these mechanisms. A slow return to normal platelet counts was likely due to a prolonged response time to antibiotics.
Conclusions: Fusobacterium infections can be associated with thrombocytopenia and hemolytic anemia.