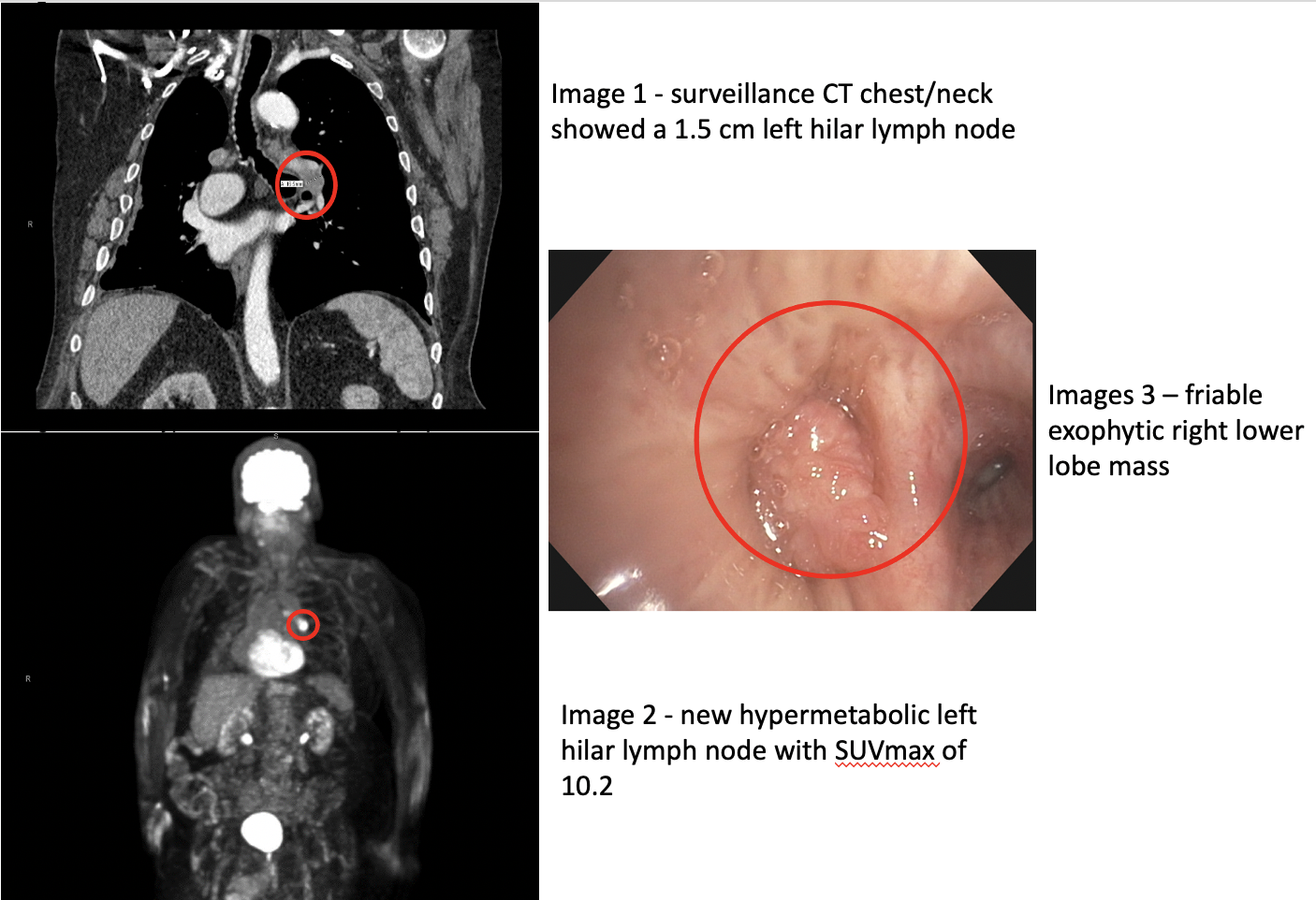
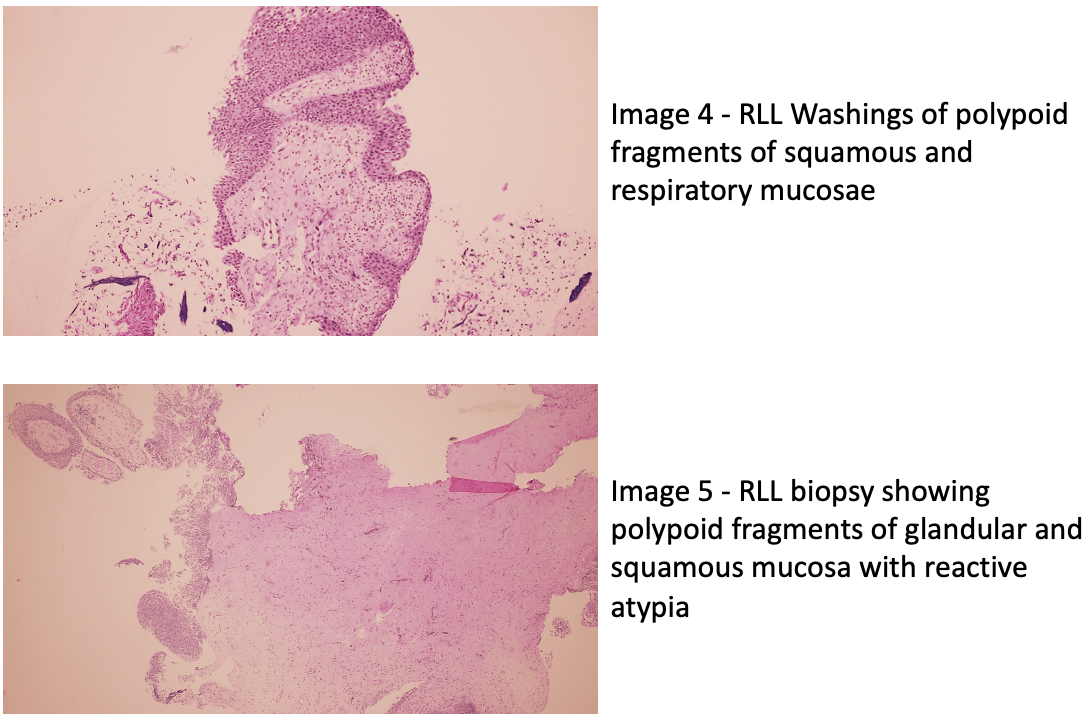
Case Presentation: A 75-year-old gentleman with a medical history significant for tonsillar squamous cell carcinoma status post resection and a previous smoker who was undergoing surveillance CT chest/neck, showed a new 1.5 cm left hilar lymph node (LHLN) (Image 1) and recurrent cytologically negative right pleural effusion. He denied any interval respiratory symptoms. PET Scan (Image 2) confirmed new hypermetabolic LHLN with SUVmax of 10.2. Bronchoscopic biopsy of LHLN showed no evidence of malignancy, while an incidental friable exophytic right lower lobe mass obstructing multiple bronchial segments was found (image 3). Biopsy results showed a papillary squamous neoplasm and bronchoalveolar lavage (BAL) was negative for malignant cells (image 4). Removal of right lower lobe (RLL) endobronchial mass using electrosurgical snare and fine needle aspiration of 11L lymph node station by EBUS, was negative for malignancy. RLL endobronchial mass was consistent with squamous cell papilloma (image 5)
Discussion: Solitary Endobronchial Papillomas (SEP) are rare, generally non-invasive tumors that are classified into squamous, glandular and mixed types. SEPs account for 0.38% of all lung tumors and though usually considered to have low malignant potential, some SEPs (particularly those of the squamous subtype) have reportedly undergone malignant transformation (1). Proposed pathogenetic mechanisms for the development of SEPs include infection with HPV, seeding from laryngeal papilloma, smoking, and foreign bodies. SEPs are a heterogeneous group of endobronchial lesions that we believe should have post-excision surveillance guidelines due to risk of malignant transformation (2).
Conclusions: SEPs are rare tumors without well-documented incidence and unpredictable clinical course, however most are benign. Early diagnosis by endobronchial biopsy remains key to differentiating malignant from benign SEPs and to prevent further complications and surgical resection (3). Studies show 63% eradication after a single procedure without recurrence of disease (4). Given the rarity of SEPs, there are no well-defined surveillance guidelines for repeat bronchoscopy. We propose that an interval bronchoscopy 3-6 months after the initial diagnosis with excision is a reasonable starting point for ensuring a timely diagnosis and treatment of recurrences given the significant theoretical risk of 8% to 40% malignant transformation. HPV has been associated with these lesions, but HPV testing with in-situ hybridization was negative in the majority of SEPs (6). We encourage more research focused on better characterization of these endobronchial tumors, which could shed light on prognosis, risks for metastasis and recurrence.